Three MRI studies have taken a closer look at the myocardium in various conditions -- healthy, infarcted, and fatally injured. First, British investigators evaluated ranges for longitudinal spin-lattice relaxation time (T1) in healthy human myocardium. In the second study, German radiologists compared an established MR imaging method, turboFLASH, to a newer technique, TrueFISP in myocardial infarction. The latter offers many advantages over turboFLASH, including a faster scan time for greater patient compliance, they said.
Patient cooperation, however, wasn't an issue for Japanese investigators, who illustrated how postmortem MRI and CT of the myocardium can guide autopsy, particularly when there is uncertainty about the cause of death.
Normal myocardium
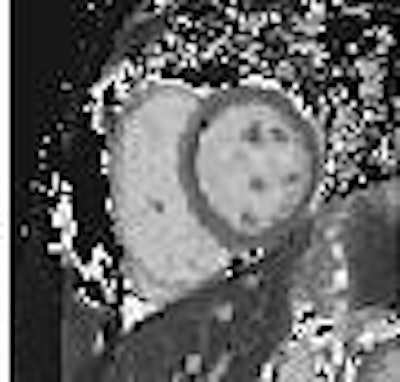
In patients with myocardial infarction, delayed gadopentetate dimeglumine enhancement on T1-weighted images identifies nonviable myocardium with high accuracy, explained Dr. Daniel Messroghli and colleagues. But T1 techniques are sometimes limited by poor spatial and/or temporal resolution. Messroghli's group suggested that a modified Look-Locker inversion-recovery (MOLLI) pulse sequence would enable myocardial T1 mapping with high spatial resolution in a single breath-hold.
"Before this technique can be used to assess T1 change in patients with myocardial disease, the normal in vivo T1 behavior of human myocardium needs to be determined," wrote the group from Leeds General Infirmary in Leeds and the University of Sheffield in Sheffield, both in the U.K., as well as Franz-Volhard-Klinik in Berlin (Radiology, March 2006, Vol. 238:3, pp. 1004-1012).
Fifteen healthy volunteers with no history of cardiovascular or systemic disease underwent two MRI exams on the same day. All studies were performed on a 1.5-tesla scanner (Gyroscan Intera CV, Philips Medical Systems, Andover, MA). The T1 mapping technique consisted of the MOLLI pulse sequence (trains), which were performed consecutively within 16-20 seconds. Study 1 consisted of a baseline MOLLI of the myocardium in the midcavity short-axis view. Study 2 was a MOLLI study in all three short-axis levels, before and after contrast administration (0.15 mmol/kg of Magnevist, Schering AG, Berlin). Study 1 and 2 were conducted on the same day. Another baseline short-axis view MOLLI test (study 3) was done 155 days later.
 |
| Representative baseline short-axis MOLLI T1 maps from all three studies in 27-year-old woman (volunteer 5). The spatial resolution (pixel size, 1.6 x 2.3 mm) is high enough to enable detection of left ventricular papillary muscles and trabeculations. Each of these maps was based on 11 steady-state free precession source MR images (3.90/1.95; flip angle, 50°; matrix, 240 x 151; section thickness, 8 mm). Figure 1. Messroghli DR , Plein, S, Higgins, DM, et al, "Human Myocardium: Single-Breath-hold MR T1 Mapping with High Spatial Resolution -- Reproducibility Study" (Radiology 2006; 238:1004-1012). |
There were 232 T1 maps with 1,362 segments available for analysis. The image quality for all segments was reviewed by Messroghli and co-author Dr. Sven Plein in consensus. Of those 1,362 images, 92.7% were rated as good for quality. The most frequently occurring artifacts were caused by respiratory (32%) or ventricular motion (31%).
"A normal range for baseline and postcontrast myocardial T1 was established (baseline mean T1 in short-axis sections, 908 msec ± 53; 95% confidence interval)," they authors wrote about their findings. "Both intra- and interobserver agreement were high (mean differences, 2.6 msec ± 6.7 and -1.1 msec ± 8.9, respectively; Bland-Altman bias analysis.... Our single breath-hold T1 mapping approach yielded interpretable image quality for 95.7% of segments."
In addition, the MOLLI technique was comparable to the saturation-recovery technique for assessing T1. The authors also found that baseline T2 values were dependent on heart rate, but postcontrast T1 values were not. They concluded that T1 mapping with high spatial resolution using MOLLI was reproducible with a clinical MR system. The next phase of research with MOLLI will have to address T1 temperature dependence, breathing artifacts, and shorter acquisition times, the group stated.
TrueFISP
Inversion-recovery turbo fast low-angle shot MR (turboFLASH) is the preferred imaging modality for myocardial infarction (MI) as it offers accurate detection and assessment. But inversion-recovery 2D single-shot true fast imaging with steady-state precession (TrueFISP) goes one better than turboFLASH, according to Dr. Armin Huber and colleagues from the Institut für Klinische Radiologie in Munich.
"This sequence allows imaging of nine slices during one breath-hold," they wrote. "The purpose of this study was to investigate the contrast-to-noise ratio (CNR) of infarction and normal myocardium for both pulse sequence techniques, to determine the diagnostic accuracy of the multislice technique in detecting MI, and to compare the area and volume of infarction with both pulse sequences techniques" (American Journal of Roentgenology, March 2006, Vol. 186:3, pp. 627-633).
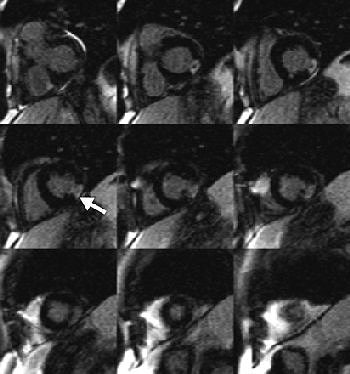 |
| Sixty-seven-year-old man with transmural myocardial infarction after occlusion of circumflex artery. Nine MR images, acquired with inversion-recovery true fast imaging with steady-state precession (trueFISP) during a single breath-hold, reveal transmural infarction (arrow) as hyperenhanced region in inferolateral segments. Huber A, Schoenberg S, Spannagl B, Rieber J, Erhard I, Klauss V, Maximilian F, Reiser M, "Single-Shot Inversion Recovery TrueFISP for Assessment of Myocardial Infarction" (AJR 2006; 186:627-633). |
For this prospective study, 43 patients with MI were enrolled. They underwent MR imaging on a 1.5-tesla scanner with eight channels and a dedicated 12-element phased-array body coil (Magnetom Sonata, Siemens Medical Solutions, Malvern, PA). Ten minutes after gadodiamide was injected (0.2 mmol/kg), a segmented inversion-recovery cine trueFISP pulse sequence was done, at a midventricular short-axis location, to establish a T1 scout. Immediately after that, the single-shot 2D inversion recovery was performed in a single breath-hold. Seventeen cardiac cycles were necessary to image nine slices. A segmented inversion-recovery turboFLASH sequence was used to cover the entire left ventricle in the short-axis view.
According to the results, 18 infarctions were located in the anteroseptal segments, 16 in the inferoseptal segments, and nine in the inferolateral segments. The trueFISP sequence showed a lower CNR than turboFLASH for viable and nonviable myocardium, the authors stated.
The mean values of signal intensity and the standard deviation of background noise are shown below:
| |||||||
| MR technique | Normal myocardium | Infarcted myocardium | Background noise |
| TrueFISP | 12.2 | 54.5 | 4.3 |
| TurboFLASH | 20.0 | 83.6 | 4.9 |
The mean SNR value for 12.6 for trueFISP with a mean imaging time of about 16 seconds. The mean SNR value for turboFLASH came in at 17.1 with a mean imaging time of around 10 minutes.
"Viable myocardium has the potential to improve its contractility after revascularization even if it has a transmural extent of 50%.... Inversion recovery trueFISP allows imaging nine slices during one breath-hold. Thus, the entire left ventricular myocardium can be covered," the authors wrote. "The single-shot technique may help to avoid respiratory motion artifacts in uncooperative patients."
They suggested that the trueFISP technique has the potential to replace turboFLASH without loss of relevant diagnostic information. MR assessment of viable myocardium with trueFISP can be combined with perfusion and stress tests for more detailed imaging.
Reversible injury
A multidisciplinary group of specialists from Tsukuba Medical Center Hospital in Tsukuba, Japan, authored a report on how postmortem MRI and CT demonstrated an interesting case of reversible injury phase myocardium without evidence of MI.
Their patient was a 46-year-old male smoker with no history of cardiac disease. He was found in his home, dead from cardiopulmonary arrest. A whole-body postmortem CT exam was done 30 minutes after death and showed diffuse ground-glass attenuation in both lungs, suggestive of pulmonary edema due to cardiac pump failure, but there was no sign of ischemic myocardium, wrote lead author Dr. Seiji Shiotani, from the department of radiology. Shiotani's co-authors are from the departments of pathology, cardiology, internal medicine, and emergency medicine.
Twelve hours after confirmation of death, the postmortem MRI was performed for a closer examination of the myocardium. T2-weighted MR imaging of the heart showed high signal intensity in the anteroseptal and apical areas relative to the remainder of the myocardium, the authors explained.
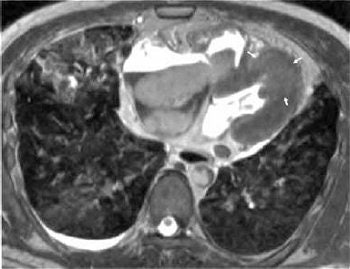
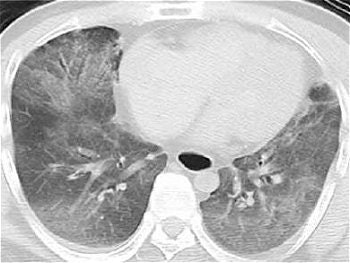 |
| Postmortem CT of the chest shows diffuse ground-glass attenuation in both the right left lower lobes. |
In addition, the heart was of normal size and a pathological examination showed no wavy fibers or edema in the left anterior descending (LAD) coronary artery territory myocardium.
"We reach the conclusion that acute plaque change in the LAD precipitated acute myocardial injury that was potentially reversible but had produced lethal pump failure (cardiogenic shock)," the group wrote (Radiation Medicine, March 2005, Vol. 23:8, pp. 563-565).
 |
| T2-weighted image of postmortem MRI of the heart shows high signal intensity (arrows) in the anteroseptal and apical areas relative to the remaining myocardium. Inhomogeneous high signal intensity in both lungs is also shown. Shiotani S, Yamazaki K, Kikuchi K, Nagata C, Morimoto T, Noguchi Y, Suzuki M, Atake S, Kohno M, Ohashi N, "Postmortem Magnetic Resonance Imaging (PMMRI) Demonstration of Reversible Injury Phase Myocardium in a Case of Sudden Death from Acute Coronary Plaque Change" (Radiation Medicine, Vol. 23, No. 8, pp. 563-565, 2005, Figure1AB). |
They considered edema to be the reason behind the high signal intensity of MRI despite the lack of microscopic evidence of edema. In addition, a decrease in the degree of cell water because of biochemical changes may have prolonged the T2 value on MRI. They concluded that, in this case, autopsy imaging with CT and MRI was useful in determining the cause of death.
By Shalmali Pal
AuntMinnie.com staff writer
June 2, 2006
Related Reading
Cardiac imaging dazzles, but radiologists can't compete alone, April 10, 2006
Heart disease in women often eludes angiography, February 2, 2006
More cardiac services don't reflect more heart disease, January 25, 2006
Myocardial contrast echocardiography accurately assesses infarct size, December 12, 2005
Copyright © 2006 AuntMinnie.com