Coronary Artery Fistula:
Clinical:
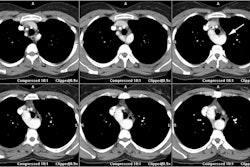
A coronary artery fistula is a rare (0.2-0.4% of congenital cardiac anomalies [2]) communication between the coronary artery and either a cardiac chamber, coronary sinus, superior vena cava, or pulmonary artery or pulmonary vein [1,2]. The lesion can be congenital or acquired- with the majority being of the congenital form [2]. The acquired lesion is most commonly seen following endocardial biopsy- especially in cardiac transplant patients. Other etiologies for acquired fistulas include coronary stent placement, CABG surgery, trauma, and chest irradiation [6].Congenital fistulous connections between the coronary system and a cardiac chamber appear to represent persistence of embryonic intratrabecular spaces and sinusoids [2]. There is no race or sex predilection [2]. A single fistula is occurs in 90% of cases (multiple fistulas are seen in 10-16% of cases) [6].
Most affected patients are asymptomatic [3] and the most common
clinical presentation is a continuous heart murmur [2]. Symptoms
depend on the location and size of the shunt as there is decreased
perfusion distal to the fistula (coronary steal phenomena
[3,7]. If symptoms develop most patients present later in
life with dyspnea and RV enlargement or dysfunction due to
progressive enlargement of the fistula and an increase in
left-to-right shunting [2]. Other presentations include fatigue,
orthopnea, chest pain, endocarditis (2-5%), arrhythmias, stokes,
angina/ischemia (secondary to a coronary steal phenomena [3]), MI,
and sudden cardiac death [2,3]. Associated cardiovascular
anomalies have been reported in 5-30% of cases [2]. On physicial
exam, there can be a loud heart murmur with a cresendo-decresendo
pattern that continues continously through systole and diastole
[6]. Patients with coronary fistulas are at an increase risk for
infective endocarditis (3-12% of patients) [6].
The right coronary artery is most commonly affected (50-60% of
cases) and the majority of symptomatic fistulas arise from the RCA
[1,2]. The fistula arises from LAD in 35-40% of cases, the left
circumflex in 5-20% of cases, and both the RCA and LCA in about 5%
[2,6]. Asymptomatic CAF's demonstrate a greater prevalence from
the LCA [2].
CAFs are classified into two categories- coronary cameral
fistulas which drain into the cardiac chamber (this is the most
common form), and coronary arteriovenous fistulas which drain to
the pulmonary or systemic circulation [6]. The fistula is usually
from the RCA to the RV (41-45% of cases); other sites of fistulous
communication include the RA (25-26% of cases), the pulmonary
artery (15-17% of cases), the coronary sinus (7%), the LA (5%),
the LV (3%), and the SVC (1%) [1,2,3]. The fistula drains into the
LA or LV in less than 10% of cases [1]. A fistula to the pulmonary
artery is most commonly from the LCA (84% of cases) and the
majority drain into the pulmonary trunk [6]. A fistula to the
coronary sinus is the CAF most frequently associated with CHF [6].
When the shunt leads to a right-sided cardiac chamber the
hemodynamics are similar to a left-to-right shunt (present in over
90% of cases) [1,2]. However, the shunt ratio is generally very
small and not detectable [2]. Myocardial perfusion can be
decreased due to a steal phenomena and can lead to myocardial
ischemia [1].
CAF's are unlikely to close spontaneously (there is only a 1-2% spontaneous closure rate) [5]. Asymptomatic CAF's can be monitored for change over time, but antiplatelet therapy and prophylactic antibiotic precautions against endocarditis are recommended [2,6]. Intervention is recommended for large fistulas or any fistula with symptoms [6]. Surgical ligation of the fistula is safe and effective with good results [2]. Transcatheter embolization and Amplatzer vascular occluders are non-surgical means of treatment for symptomatic lesions [2,5]. Indications for embolization include proximal location of the fistulous vessel, a single drain site, extra anatomic termination of the fistula away from the normal coronary arteries, older patient age, and absence of concurrent cardiac disorders that might require surgical intervention [2]. Surgery is preferred for a large CAF with high fistula flow, those with multiple communications/terminations or very tortuous pathways, significant aneurysm formation, or the presence of large vascular branches that could be accidentally embolized [2].
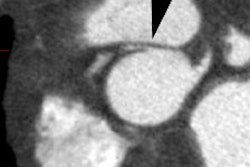
The involved vessel is usually dilated (secondary to increased blood flow) and tortuous [1].
REFERENCES:
(1) Radiographics 2006; Kim SY, et al. Coronary artery anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. 26: 317-334
(2) Radiographics 2009; Zenooz NA, et al. Coronary artery fistulas: CT findings. 29: 781-789
(3) J Nucl Cardiol 2009; Barone-Rochette G, et al. Combination or
anatomic and perfusion imaging for decision making in a
professional soccer player with a giant coronary artery to left
ventricle fistula. 16: 640-643
(4) Radiographics 2012; Shriki JE, et al. Identifying,
characterizing, and classifying congenital anomalies of the
coronary arteries. 32: 453-468
(5) Radiographics 2017; Agarwal PP, et al. Anomalous coronary
arteries that need intervention: review of pre- and postoperative
imaging appearances. 37: 740-757
(6) Radiographics 2018; Yun G, et al. Coronary artery fistulas:
pathophysiology, imaging findings, and management. 38: 688-703