Bone Imaging of Soft Tissue Abnormalities:
Mechanisms of tracer uptake:
One of the most common mechanisms of soft tissue localization of Tc-MDP is an expanded interstitial volume which produces a relative increased passive localization of the tracer. Hyperemia, which occurs following trauma or sympathectomy, can also be associated with increased soft tissue activity.
Soft tissue calcification is another reason for soft tissue uptake of Tc-MDP. Soft tissue calcification can be dystrophic, metastatic, or related to calcinosis [3]. Dystrophic calcification is the deposition of calcium salts in degraded or necrotic tissues without an underlying metabolic derangement [3]. It occurs due to a local influx of ionized calcium. Metastatic calcification occurs in non-osseous, viable tissue in the presence of severe hypercalcemia when the solubility product for calcium and phosphate is exceeded and precipitation of calcium in the extracellular space occurs. Metastatic calcification can be associated with disorders such as hyperparathyroidism [3]. Metastatic calcification usually involves joints (chondrocalcinosis) and acid secreting organs (stomach, kidneys, lungs). Alterations in pH within these tissues seems to cause selective precipitation of calcium salts at these sites. Calcinosis represents the deposition of calcium in soft tissue in the presence of normal calcium metabolism and it can be seen in disorders such as idiopathic tumoral calcinosis [3]. Transchelation of Tc-MDP may occur at injection sites where there is high local tissue concentration of metals such as iron or calcium.
Heterotopic ossification refers to the presence of bone in the soft tissues [2]. Heterotopic bone formation occurs most commonly following trauma (direct or following surgery- such as for a hip arthroplasty), but it can be neurogenic [2]. Among patients with spinal cord injury heterotopic ossification is seen about joints distal to the level of cord injury in 20-30% of patients [2]. Intense uptake is seen on bone scanning when the new bone is immature. Decreasing uptake can be seen as the bone matures. This is important because there is a lower recurrence rate of new heterotopic bone formation if surgery to remove the bone is performed when it has reached maturity.
Myositis Ossificans:
Myositis ossificans represents a post-traumatic localized form of
heterotopic ossification in the soft tissues (post traumatic
myositis ossificans is the most common subtype accounting for 75%
of cases [4]). There may be no recalled traumatic injury in up to
40% of cases [4]. It is generally seen in adolescents or young
adults and is not typically seen in children younger than 10 years
[4]. It most commonly affects the extremities and the quadriceps
femoris and nrachialis are the most commonly affected muscles [4].
Clinically, it typically presents as a painful soft tissue mass
accompanied by skin erythema and there can be systemic symptoms
such as fever, elevated ESR, and leukocytosis during the active
phase of ossifications [4]. Myositis ossificans probably
represents an exaggerated reparative response of a hematoma. There
is an early proliferative phase which occurs up to 3 weeks after
the initial trauma; an intermediate calcification phase, which
occurs 3-7 weeks after the trauma; and a mature ossification
phase, which is seen after 7 weeks [4]. Two distinct zones can be
identified in the lesion within weeks of onset: A peripheral zone
composed mostly mature bone, and a center zone which is mostly
cellular.
There are two forms of myositis ossificans observed- the more
common is a well circumscribed lesion usually adjacent to a long
bone; the other is a veil-like lesion which is generally less well
defined. Myositis ossificancs may mimic a parosteal osteosarcoma
and early there may also be an associated periosteal reaction [4],
but the latter lesion tends to be more ossified in the center and
less well defined peripherally. Additionally, there is not a
complete cleft between the lesion and the underlying bone.
Unfortunately, imaging with thallium is not helpful in
distinguishing these two lesions, as thallium accumulation has
been identified within sites of myositis ossificans [1]. Over
time, at up to 6 months, the calcified mass will become more dense
and shrunk, with a clear demarcation from the adjacent bone [4].
Other lesions is the differential for myositis ossificans
include: Osteochondroma- this lesion will communicate with the
medullary cavity of host bone; idiopathic fat necrosis (affected
patients are typically less than 6 months of age), and
dermatomyositis, but the calcifications in this disorder are more
superficial and linear.
Two other forms- nontraumatic myositis ossificans and myositis
ossificans progressiva have also been described [4]. Nontraumatic
myositis ossificans is seen most commonly in association with
burns and paralysis [4]. It more commonly occurs in adults and is
extremely common in patients with spinal cord injuries, more than
half of whom are affected with the condition [4]. When associated
with paralysis, it develops only below the level of the spinal
injury, peaking 2 months following the injury [4]. The
calcificaion in nontraumatic myositis ossificans involves
primarily connective tissues, with only secondary involvement of
skeletal muscle [4].
Myositis ossificans progressiva- also known as fibrodysplasia
ossificans progressiva, is a severely disabling heritable
connective tissue disorder characterized by congenital
malformations of the toes (hallux valgus, malformed first
metatarsal, and/or monophlangism) and progressive heterotopic
ossification at characteristic extraskeletal sites [4].
Other etiologies include: Infection, hemophilia (Factor XI deficiency), neuromuscular disorders, tetanus, and drug abuse (with I.M. injections).
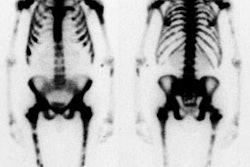
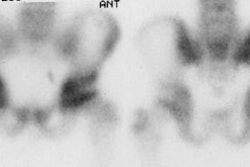
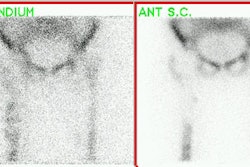
On plain film a soft tissue mass initially develops adjacent to bone following injury. Three phase bone scanning is very sensitive for the early detection of myositis ossificans. Flow and blood pool images will be positive as early as 2.5 weeks after injury, and delayed images become positive about 1 week later [2]. Ill defined floccular calcifications are seen within myositis ossificans on plain films by 4-6 weeks (but can be seen as early as 2 weeks on CT). The lesion will generally be "hot" on all three phases of bone scan at this stage. A well defined calcified mass with a radiolucent center develops by 2-3 months and is typically completely separated from the underlying bone by a radiolucent cleft (ie: myositis ossificans shows ossification in the periphery with a non-ossified radiolucent center [2]). A periosteal reaction may be seen in the sub-adjacent bone when the lesion is located juxtacortically. The lesion generally begins to decrease in size on plain films by 4-6 months and most lesions regress or may even disappear by 1-2 years. Activity on delayed scans usually peaks a few months after injury, after which time it progressively lessens and returns towards normal between 6 to 12 months [2]. The lesion may occasionally fuse with the sub-adjacent bone and mimic an osteochondroma. Although the lesion may have a very variable appearance on MRI and can sometimes be mistaken for other soft tissue masses, it is important to consider myositis ossificans if a rim of low signal intensity is seen around the lesion.
Serial bone scans have been used to monitor metabolic activity of heterotopic ossification to determine the appropriate time for surgical resection [2]. Surgery is generally delayed until the ossification has stabilized.
Note that both gallium 67 and rarely 111In-labeled WBC's have been reported to accumulate in areas of immature heterotopic ossification [2].
Etiologies of Soft Tissue Accumulation of Tc-MDP:
Common causes of soft tissue tracer accumulation include:
- Soft tissue calcification (metabolic, dystrophic)
- Radiochemical impurity: Free technetium will produce activity in the thyroid, salivary glands, and gastric mucosa.
- Trauma/ Myositis ossificans
- Rhabdomyolysis: Usually following trauma, but may follow intramuscular injections of meperidine and iron dextran.
- Inflammation: Dermatomyositis
- Infarction: MI, Cerebral, Bowel, Muscle (Sickle cell)
- Tumors: Osteosarcoma, neuroblastoma, breast, mucin-producing neoplasms, and uterine fibroids
REFERENCES:
(1) J Nucl Med 1995; Osmanagaoglu K, et al. Thallium-201 accumulation in myositis ossificans and in juxta-articular ossification. 36: 2239-42
(2) J Nucl Med 2002; Shehab D, et al. Heterotopic ossification. 43: 346-353
(3) Radiology 2007; Agarwal V, et al. Case 104: calcinosis in
juvenile dermatomyositis. 242: 307-311
(4) Radiographics 2016; Sargar KM, et al. Pediatric fibroblastic
and myofibroblastic tumors: a pictoral review. 36: 1195-1214