The team, led by Chuanhao Zhang from Capital Medical University in Beijing, found that their nomogram, a model that turns data into visual graphs for predictive purposes, showed high accuracy and agreement metrics when it came to prediction and actual outcomes. Their results were published February 9 in Thrombosis Research.
The team, led by Chuanhao Zhang from Capital Medical University in Beijing, found that their nomogram, a model that turns data into visual graphs for predictive purposes, showed high accuracy and agreement metrics when it came to prediction and actual outcomes. Their results were published February 9 in Thrombosis Research.
"Clinicians can use this predictive model to achieve risk assessment and take different treatment measures to prevent acute postoperative VTE and improve patients; quality of life effectively," Zhang and co-authors wrote.
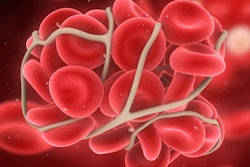
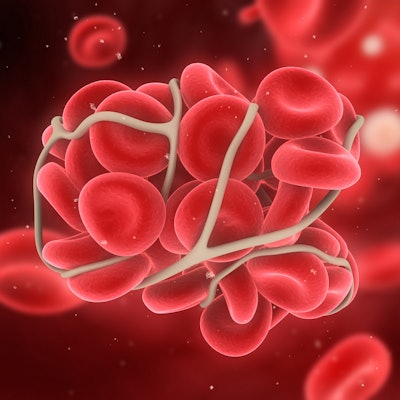
VTE has an incidence rate of about 20% in glioma patients, and it is classified as acute if it occurs within two to four weeks after surgery. The condition can cause death by pulmonary embolism or significant disability due to pain, edema, and post-thrombotic syndrome.
Zhang and colleagues sought to assess risk factors of acute VTE after glioma surgery with their nomogram. They used data collected between 2012 and 2021 from 435 patients. Duplex ultrasound was performed three to five days after surgery to define VTE; the group then combined the ultrasound findings and patient symptoms to diagnose VTE.
Zhang's team identified several risk factors for predicting acute VTE, which were used to build the nomogram: age, operation time, systemic immune-inflammation index (SII), hypertension, and diabetes mellitus.
The nomogram showed high accuracy, with area under the curve (AUC) values of 0.834 for the training set and 0.788 for the validation set. The group also reported that the Hosmer-Lemeshow goodness of fit test of the calibration curve was 3.05 (p = 0.98). This means that a high degree of agreement was shown between the prediction and actual outcome.
The researchers also performed a decision curve analysis and found that the nomogram model was helpful when the incidence of VTE was between 5% and 80% for the training set and between 5% and 50% for the validation set.
Older age was also a risk factor for VTE, which the authors suggested could be because elderly patients usually have high blood viscosity and rough intima, making them vulnerable to thrombosis. Older patients also have longer postsurgical recovery and bed-rest times, reduced activity, aggravated blood stasis, and greater susceptibility to thrombosis.
In any case, the researchers highlighted that the nomogram can help clinicians personalize and accurately identify VTE risk.
"For patients with a high risk of thrombosis assessed by nomogram, clinicians can use drugs combined with physical intervention during the perioperative period; for patients with a low risk of thrombosis, clinicians can encourage them to get out of bed and walk, which can improve patients' prognosis and quality of life," they wrote.