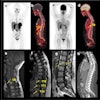
As imaging modalities go, FDG-PET produces more than its share of surprises. The technique is used most commonly to stage known cancers, of course, and to determine the malignant potential of lesions that were discovered using other modalities.
But an important additional benefit of FDG's avidity to hypermetabolism is its ability to detect unexpected malignant and pre-malignant neoplasms other than the primary tumor for which the patient was scanned, according to Dr. Harry Agress, Jr.
Agress delivered the results of a 19-month study to attendees of the 2002 Academy of Molecular Imaging conference in San Diego. Agress is the chief of the division of nuclear medicine at Hackensack University Medical Center (HUMC) in Hackensack, NJ, and a full clinical professor of radiology at the College of Physicians and Surgeons of Columbia University in New York City.
"Our study was to determine the significance of unexpected hypermetabolic foci, determined most commonly by their unusual location and less commonly by their focal measure, and relative intensity of abnormality, especially within the bowel -- for example, focal uptake within the colon as opposed to diffuse activity seen frequently as a normal variant of PET," Agress said.
The HUMC research team examined 1,800 FDG-PET scans performed in 1,650 patients between November 2000 and June 2002. The scans were performed to evaluate known or suspected malignancies of the lung, breast, head, neck, and esophagus, and to look for lymphoma, melanoma, and solitary pulmonary nodules.
The scans were performed on an ECAT Exact HR+ (Siemens Medical Solutions - Nuclear Medicine Group, Hoffman Estates, IL) with transaxial spatial resolution of 4.6-mm full width at half maximum (FWHM) at 1 cm, and a 15-cm axial field of view. An iterative reconstruction algorithm was then applied to the images. Attenuated and nonattenuated images were evaluated in three planes, and in projectional cine mode.
Patients were administered 10-15 mCi of FDG an hour before imaging. All patients had fasted 4-6 hours before the scan, and before that, had eaten a high-protein/low-carbohydrate meal to minimize cardiac activity.
The team correlated the PET images with prior CT scans at the time of interpretation. Follow-up studies such as CT, MRI, mammography, endoscopy, and image-guided biopsy were recommended on a case-by-case basis. The diagnosis was considered final only after pathologic confirmation, Agress said.
In all there were 58 unexpected findings, and 45 patients who were able to undergo follow-up. Of these 45 patients, 42 had histopathologic confirmation and three had CT correlations after the PET scan.
"Even though the images of the three patients who had CT correlations showed an obvious mass, these patients refused further evaluation and biopsy," said Agress.
Of the 42 patients with histological confirmation, 30 (71%) demonstrated malignant or pre-malignant lesions. An additional 9 (29%) patients had benign lesions; however, three of these patients had a clinically significant finding (acute/chronic cholecyctitis, pigmented villonodular synovitis, and Hashimoto’s thyroiditis), and six had clinically insignificant lesions. Three of the patients had false-positive foci with no abnormality seen at colonoscopy.
The researchers found 30 proven foci of unexpected malignant or potentially pre-malignant tumors in 26 patients. There were 18 colonic adenomas (6 villous, 4 tubovillous, and 8 tubular), 3 colonic adenocarcinomas, 2 laryngeal squamous cell carcinomas, 2 breast carcinomas (an intraductal and invasive ductal), 1 gallbladder adenocarcinoma, 1 endometrial adenocarcinoma, 1 ovarian carcinoma, 1 fallopian tube adenocarcinoma, and 1 papillary thyroid carcinoma.
"In the malignant/pre-malignant group, 24 of the 26 patients -- 92% -- were completely asymptomatic relative to their unexpected findings. One colon cancer patient had occasional mild blood streaking in the stool, when asked in retrospect, but this was not known to the referring physician. One of the laryngeal cancer patients had a negative workup for hoarseness before this study, which actually included a direct visual examination," Agress said.
The incidence of unexpected findings by the researchers was 58/1,800, or 3%. The incidence of unexpected tumors was 30/1,800, or 2%.
"Our study emphasizes the significance of the added value of PET as a whole-body scan," Agress concluded. "These findings occurred during the routine evaluation of patients with initial clinical cancer and have nothing really to do with the symptoms that brought the patient to the scan. It should be noted, however, that this study represents a very biased patient population that already has a very high incidence of cancer, and therefore may be prone to additional malignancy."
By Jonathan S. BatchelorAuntMinnie.com staff writer
December 26, 2002
Related Reading
PET/CT preferred as whole-body scan for cancer detection, December 6, 2002
Combined PET and MRI distinguish necrosis from tumor recurrence, October 29, 2002
Positron emission mammography shows promise for breast imaging, October 28, 2002
PET, SPECT given equal weight at SNM 2002, September 6, 2002
Successful PET centers require planning and persistence, July 15, 2002
Copyright © 2002 AuntMinnie.com