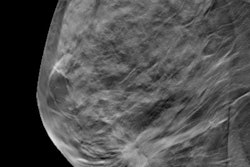
Digital breast tomosynthesis (DBT) surpasses digital mammography for reducing risk for advanced breast cancer in high-risk women with extremely dense breasts, suggests a study of over half a million women published June 14 in JAMA.
However, researchers led by Dr. Karla Kerlikowske from the University of California, San Francisco also found no significant advantages between the two modalities for reducing risk for interval invasive cancers.
"A difference may not have been observed because only 25% of interval cancers were advanced cancers and only 7.4% were among women with extremely dense breasts and at high risk," Kerlikowske and colleagues wrote.
DBT's presence in U.S. clinics has grown over the past decade, with a reported 81% of U.S. breast imaging facilities having DBT screenings available. With previous studies showing that DBT has higher accuracy than conventional mammography, researchers have discussed the potential for DBT to decrease invasive interval cancer rates. This would be an improvement over mammography for imaging women with dense breasts.
However, the study authors wrote that few studies exist that show significant decreases in interval cancer rate with DBT screening over mammograms overall or when stratified by women with dense versus nondense breasts. As a result, Kerlikowske et al wanted to find out whether DBT screening is linked to a lower likelihood of interval invasive cancer and advanced breast cancer compared with digital mammography across different breast densities.
The researchers looked at data from 504,427 women with a median age of 58 years. Out of the total, 308,141 women had only digital mammograms, 56,939 had only DBT exams, and 139,347 underwent screening with both modalities.
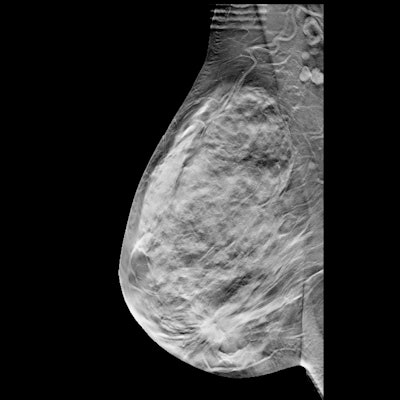
Out of the total, 3.6% (18,159) of women had extremely dense breasts and were deemed to have high risk of breast cancer. For this group, 13,291 examinations were taken via DBT and 31,300 exams through digital mammography.
The team found that advanced cancer rates per 1,000 exams were significantly lower for DBT (0.27) versus digital mammography (0.80) for women with extremely dense breasts and at high risk of breast cancer. However, the same did not go for women who had extremely dense breasts but also were low to average risk. For these women, DBT had advanced cancer rates of 0.54 per 1,000 exams while mammography had a rate of 0.42 per 1,000.
The researchers also found that for interval invasive cancer rates per 1,000 exams, DBT had a rate of 0.57 per 1,000, while mammography had a rate of 0.61 per 1,000 (p = 0.43). No significant differences in interval cancer rates were also found among exams below or above the 1.67% five-year risk threshold defined by the Breast Cancer Surveillance Consortium (BCSC).
The authors also wrote that no significant differences were found for advanced cancer rates between DBT and mammography for women at low risk, average risk, or high risk and almost entirely fatty breasts, scattered fibroglandular densities, or heterogeneously dense breasts. However, they added that digital mammography may be linked to higher false-positive recall and short-interval follow-up recommendation rates.
The study found that DBT versus mammography had significantly fewer advanced cancers (0.36 vs. 0.45), false-positive recalls (66.2 vs. 83.4), and false-positive short-interval follow-up recommendations (11.2 vs. 17.9), respectively.
"Women should be informed of the likelihood of screening failures and harms for both modalities," the authors wrote.
In an accompanying editorial, Dr. Sarah Friedewald from Northwestern University in Chicago and Dr. Lars Grimm from Duke University in North Carolina wrote that it should be feasible to have high-risk women with dense breasts screened with DBT. They added that this is due to the modality's growing presence in U.S. breast imaging facilities and its nonassociation with higher burdens for women, sans higher copays.
"However, for women at high risk but without dense breasts or women not at high risk with dense breasts, the restricted sample size of the present study precludes definitive conclusions about whether DBT is associated with decreased interval cancer rates," they wrote.