AI scoring from mammograms could help inform treatment and surveillance strategies for ductal carcinoma in situ (DCIS), according to research published February 11 in the American Journal of Roentgenology.
AI scores from a commercially available model showed independent associations with ipsilateral recurrence after breast-conserving surgery for DCIS, wrote a team led by Jung Hyun Yoon, MD, PhD, from Yonsei University in Seoul, South Korea. The researchers also reported comparable predictive performance between the AI model and existing clinical models.
“These findings support a role of the AI score on preoperative mammography in predicting the risk of ipsilateral recurrence after breast-conserving surgery for DCIS, potentially aiding proactive treatment and surveillance,” Yoon and co-authors wrote.
While between 47% and 75% of DCIS cases may not progress to invasive cancer, the standard of care is surgical excision. However, surveillance strategies have been proposed for low-risk DCIS cases, with clinical risk models and genomic assays helping to predict whether women should have surgery or undergo active surveillance.
Imaging researchers continue to explore AI’s applications in breast cancer diagnosis. Prior studies suggest that AI could provide decision support for lesion detection by assigning scores to findings. Emerging research also suggests that AI can predict breast cancer risk, including for DCIS.
The Yoon team studied associations of AI scores from a commercial system (Lunit Insight for Mammography, version 1.1.7, Lunit) for mammographic breast cancer detection and diagnosis with development of second breast cancers after DCIS treatment. It also compared predictive performance between AI and existing clinical risk models.
The retrospective study included 1,740 women who underwent surgery for DCIS between 2012 and 2017 at one of five centers. The research team reviewed medical records to identify second breast cancers, while the AI system processed preoperative mammograms.
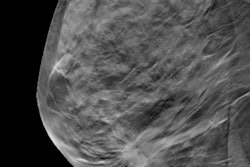
 Images of a 39-year-old who underwent screening mammography. Right craniocaudal (left) and mediolateral oblique (middle) views from preoperative mammography show suspicious grouped fine pleomorphic calcifications (arrows). After biopsy showed ductal carcinoma of situ (DCIS), patient underwent breast-conserving surgery, yielding final diagnosis of ductal carcinoma in situ (intermediate grade, hormone receptor positive). (Right) Screenshot of an output of a commercial AI tool applied to preoperative mammography. AI detected right breast lesion with score of 95% on both views (concentric colored circles). Present study’s reviewing radiologist deemed AI marking to correspond with site of DCIS.ARRS
Images of a 39-year-old who underwent screening mammography. Right craniocaudal (left) and mediolateral oblique (middle) views from preoperative mammography show suspicious grouped fine pleomorphic calcifications (arrows). After biopsy showed ductal carcinoma of situ (DCIS), patient underwent breast-conserving surgery, yielding final diagnosis of ductal carcinoma in situ (intermediate grade, hormone receptor positive). (Right) Screenshot of an output of a commercial AI tool applied to preoperative mammography. AI detected right breast lesion with score of 95% on both views (concentric colored circles). Present study’s reviewing radiologist deemed AI marking to correspond with site of DCIS.ARRS
Of the total women, 28 developed ipsilateral recurrence after breast-conserving surgery, seven developed postmastectomy ipsilateral recurrence, and 25 developed contralateral breast cancer. The researchers used an AI threshold of 73.5% or higher to denote a high risk of cancer being present on mammograms.
Postsurgery ipsilateral recurrence showed a significant independent association with AI scoring at the 73.5% or higher threshold (hazard ratio, 2.88). As well, cumulative incidence rates for post-surgery ipsilateral recurrence were higher for AI scores of 73.5% or higher than for scores below the threshold.
Cumulative incidence rates for AI scoring thresholds | |||
Measure | Below threshold | At or above threshold | p-value |
Cumulative incidence rate (five years) | 0.86% | 4.13% | < 0.001 |
Cumulative incidence rate (10 years) | 3.72% | 7.26% | < 0.001 |
The AI model achieved area under the curve (AUC) values of 0.7 and 0.66 for predicting postsurgery ipsilateral recurrence at five and 10 years, respectively. These were on par with the Van Nuys prognostic index (5 years 0.73, p > 0.99; 10 years 0.75; p = 0.66) and the Memorial Sloan Kettering Cancer Center nomogram (5 years 0.63, p = 0.82; 10 years 0.68, p > 0.99), respectively.
Finally, the team reported no associations between AI scores and other second breast cancer events in hazard models and cumulative incident rate analyses (p > 0.05).
Despite the results, the study authors noted the “suboptimal performance” of all models they evaluated in the study. They called for continued improvements to the AI model before this technology can be implemented in clinics.
However, the authors also highlighted that AI could serve as a “readily accessible preoperative tool.”
“The noninvasive information provided by the AI model could thus potentially be used to guide initial decisions regarding treatment intensity in patients eligible for breast-conserving surgery,” they wrote.
Read the full study here.