A node reporting system can successfully assess both ductal and lobular breast cancers, suggest findings published September 2 in Radiology.
Researchers led by Hee Jeong Kim, MD, from the University of Ulsan in Seoul, South Korea, found that the Node Reporting and Data System (Node-RADS) performed similarly in axillary nodal evaluation for both invasive ductal carcinoma (IDC) and invasive lobular carcinoma (ILC). However, it achieved a lower sensitivity for ILC.
“Refining Node-RADS for individual node analysis would enhance surgical planning and patient outcomes,” Kim and co-authors wrote.
While surgery is the conventional reference standard for nodal staging, recent trends point toward more use of less invasive approaches. This places emphasis on more accurate and reproducible preoperative evaluations of axillary nodal status.
Introduced by researchers in 2021, Node-RADS addresses variability in assessing and reporting lymph node involvement at CT or MRI. Radiologists can use Node-RADS to evaluate the likelihood of metastasis on a five-point scale. While the reporting and data system has performed well in previous studies, Kim and colleagues noted that imaging characteristics of breast cancer vary according to the histologic type.
Kim and colleagues studied the diagnostic performance of Node-RADS at breast MRI for predicting axillary lymph node metastasis in patients with IDC versus ILC.
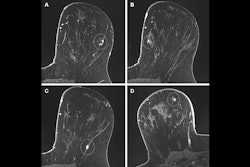
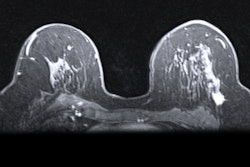
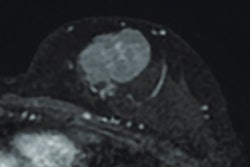
 Node Reporting and Data System (Node-RADS) true positive: images in a 39-year-old woman who presented with a palpable mass in the right breast. (A) Axial contrast-enhanced fat-suppressed T1-weighted MRI scan reveals a 27-mm irregular, heterogeneously enhancing mass in the right breast (arrows). (B) Axial contrast-enhanced fat-saturated T1-weighted image from dedicated axillary MRI reveals a prominent lymph node (arrows) in the right level I axilla, measuring 9 mm in the short axis, with focal necrosis, an irregular border, and a displaced fatty hilum. Per the Node-RADS criteria, node size was normal, but the configuration criterion yielded a sum score of 4, resulting in a Node-RADS score of 4 (i.e., high suspicion for nodal invasion). Following breast-conserving surgery, pathologic examination confirmed grade III invasive ductal carcinoma, which was estrogen receptor negative, progesterone receptor negative, and human epidermal growth factor receptor 2 positive. A sentinel lymph node biopsy, followed by axillary lymph node dissection, revealed metastasis in two of the 11 dissected lymph nodes, both of which were macrometastatic.RSNA
Node Reporting and Data System (Node-RADS) true positive: images in a 39-year-old woman who presented with a palpable mass in the right breast. (A) Axial contrast-enhanced fat-suppressed T1-weighted MRI scan reveals a 27-mm irregular, heterogeneously enhancing mass in the right breast (arrows). (B) Axial contrast-enhanced fat-saturated T1-weighted image from dedicated axillary MRI reveals a prominent lymph node (arrows) in the right level I axilla, measuring 9 mm in the short axis, with focal necrosis, an irregular border, and a displaced fatty hilum. Per the Node-RADS criteria, node size was normal, but the configuration criterion yielded a sum score of 4, resulting in a Node-RADS score of 4 (i.e., high suspicion for nodal invasion). Following breast-conserving surgery, pathologic examination confirmed grade III invasive ductal carcinoma, which was estrogen receptor negative, progesterone receptor negative, and human epidermal growth factor receptor 2 positive. A sentinel lymph node biopsy, followed by axillary lymph node dissection, revealed metastasis in two of the 11 dissected lymph nodes, both of which were macrometastatic.RSNA
The study included 1,602 women with an average age of 50.6 years who underwent breast MRI in 2017 and 2018. The study also included 1,627 breast cancers, with 25 cases being bilateral cancers. IDCs made up most cancer cases (n = 1,486), while 141 cases were ILCs.
The team reported frequencies of lymph node metastasis of 25% for IDC and 28% for ILC (p = 0.44).
Using a cutoff score of three for the Node-RADS scale showed the best performance in terms of sensitivity and specificity.
Performance of Node-RADS scale for IDCs, ILCs | |||
Measure | ILCs | IDCs | p-value |
Sensitivity | 52.5% | 71.1% | 0.02 |
Specificity | 85.1% | 86.5% | 0.71 |
Area under the curve (AUC) | 0.74 | 0.83 | 0.08 |
And using multivariable logistic regression analyses, the researchers confirmed that Node-RADS scoring is an independent predictor of axillary lymph node metastasis (odds ratio, 3.1; p < 0.001).
Scan times for this approach with a dedicated axillary MRI sequence were three minutes on a 1.5-tesla scanner and two minutes, 40 seconds on a 3-tesla scanner.
“However, acquisition time has since been decreased to under two minutes,” the researchers added.
The study authors stressed the importance of assessing both the presence of metastasis and the overall disease burden and involvement of nonsentinel nodes. And while Node-RADS scoring may have use for patients with IDC, the authors wrote that "caution is warranted when applying this system to patients with ILC," considering the lower sensitivity for these cancers.
With continued refinement and validation, Node-RADS could become central to breast cancer staging in the era of precision medicine, according to an accompanying editorial written by Vivianne Freitas, MD, from the Joint Department of Medical Imaging in Toronto, Ontario, Canada.
Freitas wrote that both diagnostic performance and the capacity to be applied across diverse patient populations and clinical settings define the utility of any imaging assessment tool.
“In this regard, the work presented by Kim et al represents a substantial advancement,” she added.
Read the entire study here.