The computerization of radiation therapy planning and treatment can be a double-edged sword, both reducing and increasing the risk of errors. But computerization does make treatment safer, according to a 10-year analysis of errors at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York City.
This information was revealed in a detailed analysis of quality assurance data published online April 11 in the International Journal of Radiation Oncology, Biology, Physics. The study shows how the frequency and nature of errors has changed with the introduction of new technologies and increased reliance on computerization.
The research team, headed by Margie Hunt, an associate attending medical physicist in the hospital's department of medical physics, determined that the error rate was less than 1% per course of treatment for 30,600 courses of external-beam radiotherapy. Treatments involving some type of manual intervention had a four times greater event risk than those relying heavily on computer-aided design and delivery.
"Increased computerization has been a significant change over the 10-year period we considered," Hunt told medicalphysicsweb. "As computer-guided data transfer, setup, verification, and treatment became more prevalent and sophisticated, we saw a decrease in the overall frequency of errors on the treatment floor. It's remarkable that this decrease occurred despite the increasing complexity of radiation oncology treatments."
A wealth of data
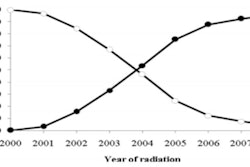
From January 2001 through December 2010, the team at MSKCC delivered approximately 597,000 x-ray or electron treatments, initiated 30,600 new external-beam radiotherapy courses, and recorded 284 errors, which are referred to as "patient events." Looking at these figures alone, this equates to an event rate of 0.05% per treatment session and 0.93% per treatment course, where the event rate per treatment course was found to vary from a high of 1.38% in 2001 to a low of 0.6% in 2009.
"Over the 10 years, the number of treatment courses per year increased but the number of events per year decreased," commented Hunt. "My opinion is that technological changes in radiation oncology, such as the increasingly widespread use of [multileaf collimation (MLC)] and [intensity-modulated radiation therapy (IMRT)], are the driving force behind this improvement."
Considering the origin
Patient events were classified into four categories according to the process step in which they originated: simulation, treatment planning, data entry/transfer, or treatment delivery. From May 2007 onward, events were recorded electronically, allowing factors such as the time of day to be considered. Prior to this, events were recorded manually.
Breaking the quality assurance data down further, the average number of events per year originating in each process step was as follows: data entry/transfer, 2.9 (10%); simulation, 3.1 (11%); treatment planning, 9.9 (35%); and treatment delivery, 12.5 (44%).
Simulation events were nearly equally distributed between documentation and measurement events. All but 7% of data entry/transfer events resulted from errors made by manual entry of field parameters. In treatment planning, monitor unit calculations accounted for approximately 75% of all events. The three predominant sources of error in treatment delivery were setup errors, incorrect use of bolus and blocks, and record-and-verify system overrides.
One particularly surprising outcome was a relationship between treatment events and the time of day, with the evening (after 5 p.m.) emerging as the most risk-prone. Possible contributing factors were thought to be the stress associated with late-day treatments of acutely ill patients or simply cumulative time pressures.
As a result of this finding, scheduling changes were made. More acutely ill patients are now scheduled for earlier treatment time slots. Educational training sessions for residents about monitor unit calculations were also conducted.
"We instigated several changes after we saw this trend and to some extent those interventions have been successful," explained Hunt. "However, our most recent data for 2011 show that we continue to have an increased event risk later in the day, so other, yet unidentified, factors may still be in force. We are actively exploring the causes and ramification of safety/QA issues like this."
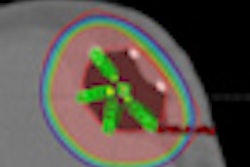
Another significant trend was the increasing frequency of events attributable to overreliance on computer systems. In 2008, the radiation oncology department recognized that it needed to add more computerized safeguards; it implemented an internally developed software program to verify proper delivery of IMRT fields by comparing the planned and delivered motion as recorded in accelerator log files.
The department had experienced an incident in which the MLC leaves incorrectly retracted to an open position at the start of treatment. This malfunction, which was identified before any patient treatment, and two other equipment malfunctions were attributed to vendor software glitches. None of the events were reproducible, and the sources of two of the three could not be identified.
Hunt is positive about the transitions that were made over the course of a decade, from decreasingly manual to increasingly computerized treatment.
"Overall, however, our data demonstrate that the benefits of computerization almost certainly outweigh the risks," said Hunt. "Continued computerization combined with other tools such as noncomputerized checklists offer the best chance of decreasing events -- at least in the near future."
Improvements for the future
Hunt stressed that work is required both at an institutional and a national level to reduce events even further.
"We will likely need to combine event reporting with other methods to identify, monitor, and reduce vulnerabilities such as failure mode and effects analysis and the Six Sigma approaches that are being discussed in the literature," she said. "A nationally recognized database is also important. If we could compare our data with others, using common terminology and reporting structure, we might learn much more about our own vulnerabilities."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.