Tumor motion due to respiration is a serious problem when it comes to ensuring that a scanned proton beam delivers the planned dose to a given target volume. Now, software simulating the delivery of a scanning proton beam to a moving lung tumor is resolving this problem.
Simulation software uses patient-specific image and plan data to estimate the effects of motion on dose during scanned-beam proton therapy. It is described in a study undertaken by German and Canadian researchers published in the October 21 issue of Physics in Medicine and Biology (2011, Vol. 56:20, pp. 6563-6582).
"Our simulation software uses patient-specific motion and treatment plan data in order to realistically estimate the effects of motion on the dose during irradiation by a scanning proton beam," Kim Kraus, a doctoral student in medical physics at the German Cancer Research Center (DKFZ), told medicalphysicsweb. "Previous studies have used periodically moving water phantoms, or applied periodic motion models to patient data, but typical breathing motion is not limited to these models."
Patient-specific approach
The team performed a comprehensive analysis of data gathered from two patients. In each case, patient motion data were derived from a 4D CT scan comprising 10 respiratory phases. The exhale phase was used as a reference against which motion in subsequent respiratory phases could be measured. Treatment planning data were generated using DKFZ's KonRad software, whereby the clinical target volume was expanded to an internal target volume to encompass tumor motion. The prescribed dose to the internal target volume was 60 Gy.
With the patient-specific data acquired, the next step was to run the simulation. "We scan through the target volume with the treatment beam while keeping track of the time throughout the entire dose delivery," explained Kraus. "We then calculate dose influence matrices for the 10 breathing phases. For each proton spot being delivered, we calculate the breathing trajectory for each voxel of the target volume and accumulate the dose along this breathing trajectory."
Assessing interplay effects
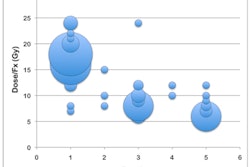
The team assessed the effects of fractionation, different beam arrangements (one beam versus three beams), and volumetric rescanning. Single fraction delivery was found to result in severely distorted dose distributions due to interplay effects for all investigated patients and beam arrangements.
Baseline shift variations for single-fraction delivery reduced the dose to the clinical target volume by up to 14.1 Gy. Local overdosage of 12.3% compared to the statically delivered dose remained for breathing period variations, the researchers reported.
"Up to 23% underdosage and up to 29% overdosage to the clinical target volume compared with the prescribeddose of 60 Gy were noted," commented Kraus. "Delivering the prescribed dose in 30 fractions reduced interplay effects by up to 33% compared with single-fraction delivery. However, local under- and overdosages within the target volume as well as the lung remained."
The team believes that volumetric rescanning -- where the internal target volume is scanned with the proton beam several times with a certain fraction of the prescribed dose -- has the potential to average out the detrimental effects to the dose distribution, but they caution that for different motion data and tumor volumes, the benefits of rescanning will vary.
"The largest influence on the dose distribution is caused by variations of the baseline, meaning the entire breathing trajectory is shifted by a certain amount," explained Kraus. "The second most significant parameter is the breathing amplitude. Both of these factors let the target position deviate from the planned position. Less pronounced was the influence of the breathing period and different initial phases of the breathing trajectory. However, the dosimetric effects of these parameters are not negligible."
To overcome interplay effects, Kraus and colleagues Uwe Oelfke, PhD, group leader of research of DKFZ's department of medical physics in radiation oncology, and Emily Heath, PhD, assistant professor of biomedical physics at the Yeates School of Graduate Studies at Ryerson University, concluded that other motion mitigation techniques such as gating or tracking should be investigated.
"We have already started to investigate gating as well as combined gating and rescanning," said Kraus. "In future we could also think of using the software to model the effects of motion for treatment devices other than those based on a synchrotron."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.