Even in people without a history of cardiovascular disease, higher left-to-right ventricular and atrial volumes suggest increased risk of heart failure, atrial fibrillation, and even death, researchers have reported.
The findings could help clinicians categorize patients' cardiac risk with more accuracy, wrote a team led by Malak Hoballah, MD, of Johns Hopkins University in Baltimore. The study results were published August 19 in Radiology.
"[Our findings are] important clinically as, on its basis, the risk of cardiac events in patients who are deemed to have normal volumes could be restratified by evaluating chambers interdependently," the study authors noted.
The clinical significance of left-to-right heart chamber volume imbalances -- even when individual chamber volumes are within "normal" ranges -- has been unclear, Hoballah's team explained. The group assessed whether volumetric imbalance between the left and right ventricles and atria assessed with cardiac MRI indicates risk of cardiac events in people without a history of cardiovascular disease (CVD).
The investigators did this via a secondary analysis of data from 4,073 patients (median age, 61) who participated in the Multi-Ethnic Study of Atherosclerosis (or MESA, which was conducted between July 2000 and July 2002). These patients underwent cardiac MRI and were free of CVD at baseline. The team defined left-to-right ventricular volume ratio (LRVR) at end diastole and left-to-right atrial volume ratio (LARA) at end systole. LRVR values were considered balanced between the range of 0.8 and 1.3; low at <0.8; and high at >1.3. LARA values were classified into low (≤2) and high (>2) measures. The group used Cox regression models to explore any associations of LRVR and LARA with heart failure, atrial fibrillation, and death.
Hoballah and colleagues reported the following:
- In follow-up, 239 (5.9%) study participants developed heart failure, 772 (19%) developed atrial fibrillation, and 906 (22.2%) died.
- A high LRVR was associated with increased risk of heart failure (hazard ratio [HR], 2.54; p< 0.001), atrial fibrillation (HR, 1.57; p = 0.001), and death (HR, 1.62; p < 0.001) compared with those with a balanced LRVR.
- In those with normal right ventricle and left ventricle volumes, high LRVR still predicted heart failure (HR, 1.99; p = 0.04), atrial fibrillation (HR, 1.55; p = 0.04), and death (HR, 1.57; p = 0.02).
- High LARA predicted heart failure (HR, 1.99; p < 0.001) and atrial fibrillation (HR, 1.41; p < 0.001) after adjustment for traditional risk factors, particularly affecting outcomes in patients with an LRVR of less than 1.3.
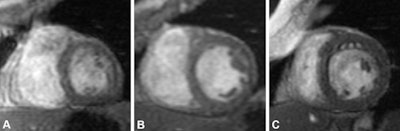 Example of noncontrast short-axis cardiac MRI scans of the heart at end diastole in participants with varying left-to-right ventricular volume ratios (LRVRs). (A) Image in a 78-year-old male with right ventricle (RV) predominance (LRVR < 0.8) with an LRVR of 0.56, left ventricular end-diastolic volume indexed to body surface area (LVEDVi) of 44.44 mL/m2, and right ventricular end-diastolic volume indexed to body surface area (RVEDVi) of 79.88 mL/m2. (B) Image in a 65-year-old male with balanced left ventricle (LV)–RV with an LRVR of 1, LVEDVi of 62.07 mL/m2, and RVEDVi of 62.07 mL/m2. (C) Image in a 74-year-old female with LV predominance (LRVR > 1.3) with an LRVR of 2.06, LVEDVi of 94.81 mL/m2, and RVEDVi of 46.1 mL/m2. Images and caption courtesy of the RSNA.
Example of noncontrast short-axis cardiac MRI scans of the heart at end diastole in participants with varying left-to-right ventricular volume ratios (LRVRs). (A) Image in a 78-year-old male with right ventricle (RV) predominance (LRVR < 0.8) with an LRVR of 0.56, left ventricular end-diastolic volume indexed to body surface area (LVEDVi) of 44.44 mL/m2, and right ventricular end-diastolic volume indexed to body surface area (RVEDVi) of 79.88 mL/m2. (B) Image in a 65-year-old male with balanced left ventricle (LV)–RV with an LRVR of 1, LVEDVi of 62.07 mL/m2, and RVEDVi of 62.07 mL/m2. (C) Image in a 74-year-old female with LV predominance (LRVR > 1.3) with an LRVR of 2.06, LVEDVi of 94.81 mL/m2, and RVEDVi of 46.1 mL/m2. Images and caption courtesy of the RSNA.
One of the "most remarkable" findings in the study is "the independent prognostic value of LRVR for cardiac events -- even in participants with left and right ventricular volumes within normal ranges," wrote Farah Cadour, MD, of the University of Toronto in Canada, and colleague Prof. Jean-Nicolas Dacher of Rouen-Normandy University Hospital in France, in an accompanying editorial.
More research is needed, the two noted.
"The next step would therefore be to confirm these results with echocardiography, which is a widely available and routinely used first-line modality," they concluded. "If successfully confirmed, these results would have a large global impact on early identification of patients who would be at higher risk of cardiac events and would need close monitoring."
Click here for the full study.