An AI model based on gross total resection of a noncontrast-enhanced tumor (GTR-NET) data culled from MRI shows promise for predicting overall survival in patients with a particularly virulent brain cancer, researchers have reported.
The findings could help clinicians better assess outcomes for patients with a cancer called isocitrate dehydrogenase (IDH) wild-type glioblastoma, according to a team led by Hye Hyeon Moon, MD, of the University of Ulsan in Seoul, Korea.
"[Our study found that] GTR-NET is an independent prognostic marker for longer overall survival in IDH-wildtype glioblastoma," the group wrote in an article published May 6 in Radiology.
IDH-wildtype glioblastoma often features a noncontrast-enhanced tumor component on MR imaging, and the extent of the tumor's resection can serve as a prognostic marker, the investigators wrote. To assess outcomes based on GTR-NET, Moon and colleagues developed a "real-world" survival AI model that incorporated GTR-NET data from MRI exams, conducting a study that included 201 patients with IDH-wildtype glioblastoma (data were taken from a registry that covered March 2017 to October 2020; these patients made up the model's training set).
A set of 352 patients whose data were recorded between March 2017 and January 2023 made up an external validation cohort. Study participants underwent both preoperative and postoperative MRI that included T1-weighted, T2-weighted, fluid attenuated inversion recovery (FLAIR), three-dimensional contrast-enhanced T1-weighted, and diffusion-weighted imaging protocols.
Moon's team categorized patients into the following prognostic groups: Gross total resection of a noncontrast-enhanced tumor; gross total resection of a contrast-enhanced tumor; and no gross total resection.
The investigators reported the following:
- GTR-NET was associated with a better prognosis, with a median overall survival of 32.6 months.
- When gross total resection was not achieved, patients' prognosis was poorer: Those younger than age 60 showed a median overall survival of 23.4 months; those 60 years or older and positive for the MGMT gene showed a median overall survival of 19.1 months; and those 60 years or older without the MGMT gene showed a median overall survival of 10.7 months.
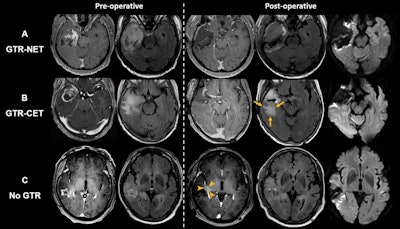 Axial MRI scans show extent-of-resection groups for (A) gross total resection (GTR) of both contrast-enhanced tumor (CET) and noncontrast-enhanced tumor (NET) (GTR-NET), (B) GTR of CET but NET remained (GTR-CET), and (C) no GTR. Scans show (B) residual T2 and fluid-attenuated inversion recovery (FLAIR) high-signal infiltrative tumor (arrows) and (C) residual CET around the surgical cavity (arrowheads). Diffusion-weighted imaging (right-side column) was used to differentiate residual T2-weighted or FLAIR signal
Axial MRI scans show extent-of-resection groups for (A) gross total resection (GTR) of both contrast-enhanced tumor (CET) and noncontrast-enhanced tumor (NET) (GTR-NET), (B) GTR of CET but NET remained (GTR-CET), and (C) no GTR. Scans show (B) residual T2 and fluid-attenuated inversion recovery (FLAIR) high-signal infiltrative tumor (arrows) and (C) residual CET around the surgical cavity (arrowheads). Diffusion-weighted imaging (right-side column) was used to differentiate residual T2-weighted or FLAIR signal
hyperintensity as a result of NET from cytotoxic surgery-induced changes. Images and caption courtesy of the RSNA.
"An important finding of our study is that in [our] model, GTR-NET stands out as the primary determinant for patient risk categorization, underscoring the clinical significance of supramaximal resection," they concluded. "Considering that surgery is the sole prognostic factor actively pursued by clinicians, we recommend achieving maximum or complete resection of NETs if possible."
The complete study can be found here.








![Images depict axial MRI scans in a 50-year-old premenopausal female patient with biopsy-proven 12-mm invasive lobular cancer in the lower outer quadrant of the left breast. Upper images are subtracted dynamic contrast-enhanced (DCE) MRI scans from the first and second postcontrast acquisitions. Lower images are ultrafast MRI scans obtained within 24 hours after the DCE study (four consecutive subtracted dynamic frames from time points [T] 6–9). There is marked background parenchymal enhancement (BPE) on the DCE MRI scans. Thus, the known cancer (arrow) is barely visible; it exhibits only slightly stronger enhancement than the normal fibroglandular tissue, which results in low conspicuity. At ultrafast MRI there is less BPE, and still the cancer is barely visible because it starts to enhance simultaneously with the BPE. The conspicuity of the cancer is even reduced compared with the DCE series. Both of the readers missed this cancer on both the DCE and ultrafast MRI scans.](https://img.auntminnie.com/mindful/smg/workspaces/default/uploads/2025/05/2025-05-06-rsna-ultrafast-dce-mri-breast.Gzvq76udFr.jpg?auto=format%2Ccompress&fit=crop&h=167&q=70&w=250)












