An algorithm based on MRI features could help clinicians predict liver cancer recurrence after patients have undergone liver resection, researchers have found.
The findings could translate into better patient outcomes, wrote a team led by Hanyu Jiang, PhD, of West China Hospital, Sichuan University, in Chengdu, China. The study results were published November 7 in Radiology.
"Identifying patients at high risk for advanced-stage hepatocellular carcinoma recurrence after liver resection may improve patient survival," the group noted.
Liver resection is a common treatment for hepatocellular carcinoma, but its long-term effect can be limited by the frequent recurrence of the disease, according to the researchers. That's why patients at high risk for advanced-stage recurrence could "benefit from adjuvant therapies and a more intensive postsurgical surveillance strategy for extrahepatic metastases," they wrote.
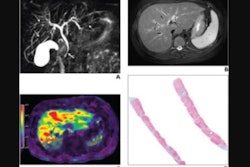
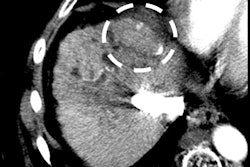
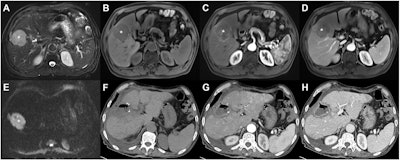 Preoperative axial extracellular contrast agent-enhanced (A-E) MRI and (F-H) follow-up CT images in a 71-year-old male patient with chronic hepatitis B and a serum neutrophil count of 4.2 × 109/L. A 5.6-cm mass with a 1.9-cm satellite nodule was detected in segments V and VIII. (A) The mass (asterisks, A-E) shows mild-to-moderate hyperintensity on T2-weighted images, (B) hypointensity on T1-weighted noncontrast-enhanced images, (C) less than 50% hyperenhancement on late arterial phase images, (D) nonperipheral washout and incomplete enhancing capsule on portal venous phase images, and (E) marked diffusion restriction on diffusion-weighted images (b = 800 sec/mm2). The mass was confirmed at histopathologic analysis as moderately differentiated hepatocellular carcinoma with microvascular invasion. With an advanced-stage recurrence after resection score of 19.8 points (4.2 + 5.6 + 10), this patient was assigned to the high-risk group (≥15 points) for advanced-stage recurrence. At follow-up, (F) noncontrast-enhanced, (G) arterial phase, and (H) portal venous phase CT images acquired at day 70 after surgery show multifocal intrahepatic recurrence and tumor thrombus in the left portal vein (black arrow, H). Images and caption courtesy of the RSNA.
Preoperative axial extracellular contrast agent-enhanced (A-E) MRI and (F-H) follow-up CT images in a 71-year-old male patient with chronic hepatitis B and a serum neutrophil count of 4.2 × 109/L. A 5.6-cm mass with a 1.9-cm satellite nodule was detected in segments V and VIII. (A) The mass (asterisks, A-E) shows mild-to-moderate hyperintensity on T2-weighted images, (B) hypointensity on T1-weighted noncontrast-enhanced images, (C) less than 50% hyperenhancement on late arterial phase images, (D) nonperipheral washout and incomplete enhancing capsule on portal venous phase images, and (E) marked diffusion restriction on diffusion-weighted images (b = 800 sec/mm2). The mass was confirmed at histopathologic analysis as moderately differentiated hepatocellular carcinoma with microvascular invasion. With an advanced-stage recurrence after resection score of 19.8 points (4.2 + 5.6 + 10), this patient was assigned to the high-risk group (≥15 points) for advanced-stage recurrence. At follow-up, (F) noncontrast-enhanced, (G) arterial phase, and (H) portal venous phase CT images acquired at day 70 after surgery show multifocal intrahepatic recurrence and tumor thrombus in the left portal vein (black arrow, H). Images and caption courtesy of the RSNA.
"Identifying these patients may help inform personalized decision-making and improve survival," the team explained.
Jiang and colleagues conducted a study that included 532 patients who underwent preoperative contrast-enhanced MRI before resection for early- to intermediate-stage hepatocellular carcinoma between December 2011 and April 2021. To develop a predictive model -- which the team dubbed advanced stage recurrence after resection, or ASRAR -- the investigators identified clinical, laboratory, imaging, pathologic, and surgical variables for the predictive model training set (of the 532 patients, 302 were included in the training set and 128 in a test set).
The researchers reported advanced-stage liver cancer recurrence in 38 of the 302 training set patients (12.6%) and 15 of the 128 test set patients (11.7%). They also found the following:
- Arterial phase hyperenhancement proportion on MRI scans, serum neutrophil count (109/L), and tumor size (in centimeters) were associated with advanced-stage recurrence, with an odds ratio of 1.16 (with 1 as reference).
- The ASRAR model showed better prediction performance for advanced-stage recurrence than four conventional staging systems ranked by 2-year C-indexes (i.e., the Barcelona Clinic Liver Cancer system; the Union for International Cancer Control system; American Joint Committee on Cancer system; and the unresectable hepatocellular carcinoma prognostic index), at 0.82 compared to an average of 0.63 (C-index values over 0.7 indicate an effective model).
- Patients at high risk for liver cancer recurrence as defined by the model showed increased advanced-stage recurrence and worse all-stage recurrence-free survival, advanced-stage recurrence-free survival, and overall survival than patients at low risk for recurrence.
The ASRAR model shows promise, but more research is needed, according to the authors.
"Future multicenter prospective studies enrolling participants with more diverse etiology and treatments are warranted to refine the ASRAR score, and to validate its uses as a potential clinical decision-making tool," they concluded.
The complete study can be found here.