MRI without oral contrast is useful for evaluating pregnant patients suspected of having appendicitis and should be used as an adjunct imaging test in their clinical workup, according to a study published in the April issue of Radiology.
Adding an MRI scan when appendicitis was suspected in pregnant patients decreased the negative laparotomy rate for these patients by 47%, without a significant change in perforation rates, concluded researchers from Cambridge Hospital in Massachusetts and Yale University School of Medicine.
MRI also achieved high sensitivity, specificity, positive predictive value, and negative predictive value, wrote lead author Dr. Elliot Rapp, from Cambridge's department of internal medicine, and colleagues (Radiology, April 2013, Vol. 267:1, pp. 137-144).
Increasing use
Acute appendicitis is the most common nonobstetric condition that requires surgery in pregnant women, according to the authors. But clinicians face a dilemma: Observing patients without performing an intervention can lead to an increased perforation rate, while performing surgery on the basis of initial clinical evaluation can lead to a higher negative laparotomy rate -- and previous studies have found the two rates to be inversely proportional.
In theory, imaging could lead to reductions in both rates by allowing clinicians to determine more precisely which patients should proceed to surgery. However, CT is avoided in pregnant women due to concerns about radiation's effect on the fetus, leading many physicians to turn to ultrasound and MRI. Few studies have examined whether the use of MRI will affect a facility's negative laparotomy and perforation rates.
MRI use in pregnant patients suspected of having acute appendicitis is on the rise, Rapp and colleagues noted. In a 2007 survey of 85 U.S. academic centers, 80 facilities (94%) used MRI on pregnant women to investigate abdominal pain, with 57 respondents (67%) adding that they do not administer gadolinium during pregnancy (Jaffe et al, American Journal of Roentgenology, November 2007, Vol. 189:5, pp. 1128-1134).
Several other studies have reported sensitivities and specificities between 80% and 100%, showing how MRI can be helpful in excluding appendicitis in patients whose ultrasound scans were inconclusive.
The current study included 267 pregnant patients who underwent either surgery (82 women) or MRI (217 women) due to suspected appendicitis between January 1996 and August 2011.
The study also divided the participants into two groups: A pre-MRI cohort was created for the years 1996 to 2003, before MRI was utilized for this clinical application, and a post-MRI group was established for 2004 to 2011, when the modality became more prominent in clinical workups.
The mean age of patients undergoing surgery in the pre-MRI cohort was 30 years (± 6 years), compared with a mean age of 26 years (± 6 years) in the post-MRI group. For the entire study population, there were 50 positive appendectomies, 32 negative appendectomies, and 12 perforations.
Exams were performed on 1.5-tesla MRI systems (Avanto or Espree, Siemens Healthcare; Excite HD or Signa, GE Healthcare) with the patient in a supine position using a body phased-array coil. No oral, rectal, or intravenous contrast material was administered.
MRI usage
Thirty-one patients received an MRI scan as the first or only imaging procedure. One patient underwent MRI after a positive ultrasound scan, the only case of a false-positive MRI scan in the study.
The other 185 patients received MRI exams after appendicitis could not be determined through ultrasound. MRI was able to visualize the appendix in 70 (32%) of the 217 cases.
Among patients in the pre-MRI cohort, ultrasound was performed on 26 (84%) of 31 patients who ultimately underwent surgery. With ultrasound, there were three true-positive results and no false positives. There were four cases in which appendicitis could not be excluded by ultrasound, and follow-up MRI scans were negative. None of those patients required surgery.
Three CT exams were performed after indeterminate ultrasound scans. Two were false positive and one was a true-positive result. One CT examination was performed after an inconclusive ultrasound and a positive MRI. Both CT and MRI were true positive.
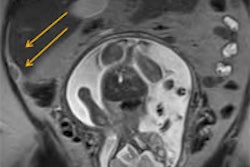
In the post-MRI cohort, ultrasound was performed for 41 (80%) of 51 patients who went to surgery. There were 12 true-positive ultrasound results, with no patients requiring an MRI. One ultrasound image showed a normal appendix, but the follow-up MRI exam displayed a perforated appendix with abscess. In addition, one ultrasound suggested a partial appendicitis, but the MRI indicated the condition involved the entire appendix.
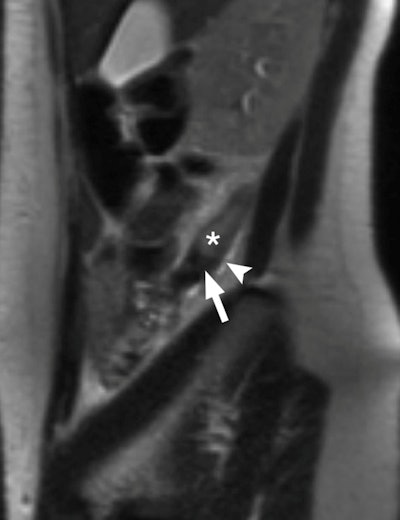 |
| True-positive MRI of a 24-year-old pregnant woman with surgically proved appendicitis. Sagittal T2-weighted single-shot fast spin-echo through appendix (*) shows dilated appendix that measures up to 12 mm. High-signal-intensity fluid and edema (arrowhead) are present around the appendix. Low signal intensity within the lumen toward the base of the appendix (arrow) may represent an appendicolith. Image courtesy of Radiology. |
Outcome changes
As for MRI's influence on patient outcomes, there was a negative laparotomy rate of 55% (17 of 31 patients) in the pre-MRI cohort, compared with 29% (15 of 51) in the post-MRI cohort, representing a 47% decrease when MRI was used regularly in suspected appendicitis cases.
The appendix perforation rate was 21% (three of 14) in the pre-MRI group, compared with 26% (nine of 35) in the post-MRI cohort. The decline in the negative laparotomy rate was statistically significant, but the change in perforation rate was not, Rapp and colleagues reported.
| MRI in the diagnosis of appendicitis | |||||
| Sensitivity | 89% (17 of 19) | ||||
| Specificity | 97% (187 of 193) | ||||
| Positive predictive value | 74% (17 of 23) | ||||
| Negative predictive value | 99% (187 of 189) | ||||
"MR imaging without oral contrast material is a valuable diagnostic tool for evaluating pregnant patients suspected of having appendicitis," the authors concluded.
They cited several limitations of the study, including the fact that not all patients with abdominal pain underwent MRI.
"Some may have been discharged without imaging or after a negative [ultrasound] examination," they wrote. "Nevertheless, we believe that nearly all pregnant patients evaluated for appendicitis were captured by our study."