Although hysterectomy is the definitive treatment for adenomyosis, uterine artery embolization (UAE) can improve symptoms such as bleeding and pain. But many women with adenomyosis have co-existing pelvic disease, making it difficult to determine if UAE truly has a beneficial effect on adenomyosis. Researchers from Washington, DC, performed an MRI study in adenomyosis-only patients to correlate imaging features with clinical symptoms.
"The clinical diagnosis of adenomyosis is difficult because between 60% and 80% of women with adenomyosis have coexisting pelvic disease, the most common being fibroids, which are present in 35% to 55% (of cases)," wrote Dr. Yuri Kitamura and colleagues in the women's imaging supplement of the American Journal of Roetgenology (March 2006, Vol. 186:3, pp. 855-864).
Kitamura lead this study along with co-authors from Georgetown University Hospital and the Lombardi Cancer Center in Washington, DC. Kitamura is now at the Kobe University Graduate School of Medicine in Hyogo, Japan.
Their patient population consisted of 31 women (mean age of 44.6 years) with pure or dominant adenomyosis, which was confirmed with a baseline MRI performed two months before UAE.
UAE was done either with polyvinyl alcohol particles or trisacryl gelatin microspheres. Three to 12 months after UAE, patients were asked to fill out a questionnaire about their symptoms.
Post-UAE MRI was performed on a 1.5-tesla system (Magnetom Vision, Siemens Medical Solutions, Malvern, PA; or Signa, GE Healthcare, Chalfont St. Giles, U.K.). The scanning protocol included axial T2-weighted single-shot FSE relative to the pelvis; orthogonal T2-weighted single-shot FSE relative to the uterus; and sagittal T1-weighted fat-saturated spoiled gradient-echo imaging with and without contrast (0.1 mmol/kg of Magnevist, Berlex Imaging, Wayne, NJ).
Two experienced MR imagers reviewed the T1-weighted, T2-weighted, and delayed gadolinium-enhanced T1-weighted images of the uterus before and after UAE. Adenomyosis enhancement was assessed by comparing precontrast and the third postcontrast fat-suppressed T1-weighted images.
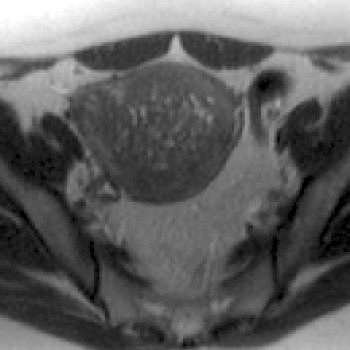 |
| A 44-year-old woman with asymmetric diffuse adenomyosis. T2-weighted axial image obtained before UAE showed asymmetric diffuse thickening of junctional zone with multiple high-signal-intensity foci within that zone, which is compatible with adenomyosis. |
"Because the imaging features of adenomyomas and fibroids may overlap, features favoring the diagnosis of adenomyosis may include the following: a lesion with poorly defined borders, elliptic shape extending along the endometrium, and minimal mass effect relative to size," the authors wrote.
For the initial analysis, the results in 19 patients were used. Those results showed a 25.1% decrease in mean uterine volume after UAE and 13.7% decrease in mean junctional zone thickness. Of the 19 patients, 14 showed at least one area of devascularization within the adenomyosis.
In terms of clinical symptoms, 16 of the 18 patients who completed the questionnaire three months after UFE reported an improvement in symptoms. In the 16 patients, the distribution pattern of adenomyosis was mostly asymmetric diffuse. Finally, 11 of 16 patients had regions of devascularization.
Eleven of 19 patients completed the questionnaire after one year. Overall, 10 reported clinical improvement and eight of these had regions of devascularization.
The authors surmised that their study showed that uterine volume decreased by 25.1%, junctional zone thickness decreased by 13.7%, and 94.4% of the 19 patients showed symptomatic improvement after three months. In a subgroup of 17 patients, uterine volume decreased by 13.7%, junctional zone thickness by 13.3%, and symptoms improved in 88.9% of the cases.
 |
| Same patient. Above, T2-weighted sagittal image obtained four months after treatment shows decrease in uterine size and junctional zone thickness, and new area of decreased signal intensity in region of adenomyosis. Below, contrast-enhanced T1-weighted sagittal image obtained during same study shows nonenhancement of this area, which signified devascularization in region of adenomyosis. Kitamura Y, Allison SJ, Jha RC, Spies JB, Flick PA, Ascher SM, "MRI of Adenomyosis: Changes with Uterine Artery Embolization" (AJR 2006; 186:855-864). |
 |
"Because increased endometrial cavity size contributes to bleeding with adenomyosis, reduction in total uterine size with an associated reduction in endometrial size after UAE may explain, in part, alleviation of symptoms," they wrote. Additionally, decrease in junctional zone thickness was significant because increased microvessel density associated with adenomyomas is generally observed in the junctional zone-myometrium.
The authors acknowledged that they had a small sample size of patients, despite four years of recruitment. While the study did illustrate the short-term benefits of UAE for treating adenomyosis, the long-term durability of the procedure in these patients still needs to be evaluated, they stated.
One of Kitamura's co-investigators, Dr. James Spies, also co-authored several UAE papers that will be presented at the upcoming 2006 Society for Interventional Radiology (SIR) meeting in Toronto. Topics include clinical and imaging outcomes after repeat UAE (scientific session abstract 144), as well as the economic impact of UAE (abstract 145).
By Shalmali Pal
AuntMinnie.com staff writer
March 15, 2006
Related Reading
UAE beneficial over long term, latest registry data shows, February 4, 2006
Existing research lacking dollars-and-cents assessment of uterine fibroids, November 23, 2005
Diffusion-weighted MR noninvasively monitors uterine fibroid therapies, September 9, 2005
Copyright © 2006 AuntMinnie.com