Recurrent lumbar disk herniation occurs in 5% to 11% of patients treated with surgery. One potential risk factor for a failed diskectomy is the size of the annular defect; another is disk herniation volume. Now Swiss investigators have recommended adding the degree of degeneration to the list of risk factors.
"The present study results demonstrate that low-grade disk degeneration (grades I-III) is an important risk factor for recurrent disk herniation," wrote Dr. Claudio Dora, Dr. Marius Schmid, and colleagues. "This is important to consider when patients are informed about the potential outcome after diskectomy" (Radiology, May 2005, Vol. 235:2, pp. 562-567).
Dora is from the Center for Spinal Surgery at the University of Zurich, Balgrist Hospital, while Schmid is from the department of radiology. Other co-authors are from Balgrist, as well as the University of Bern in Switzerland.
This retrospective study included 30 consecutive patients who had undergone surgical treatment for recurrent disk herniation. The control group consisted of 30 patients who had undergone primary diskectomy.
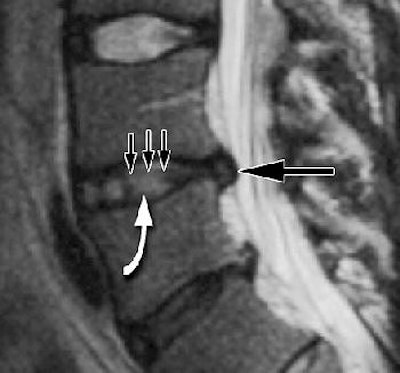
MR imaging was performed on a 1-tesla unit (Expert, Siemens Medical Solutions, Erlangen, Germany) using a dedicated receive-only spinal coil. The imaging sequences included sagittal T1-weighted spin-echo and transverse T2-weighted turbo spin-echo. Disk degeneration was assessed on the latter images using a five-point grading system, with grade I indicating no degeneration and grade V a collapsed hypointense disk.
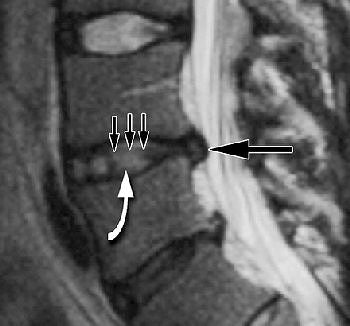 |
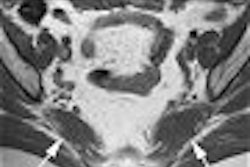
| Grade II disk degeneration with recurrent disk herniation. T2-weighted sagittal MR image (5000/130) obtained in 41-year-old man in study group with lumbar disk herniation (long black arrow) at the L4-5 level before primary diskectomy. Disk degeneration was rated as grade II because an inhomogeneous bright nucleus pulposus (white arrow) with hypointense bands (short black arrows) was seen. Figure 3, Dora C, Schmid MR, Elfering A, Zanetti M, Hodler J, Boos N, "Lumbar disk herniation: Do MRI findings predict recurrence after surgical diskectomy?" Radiology 2005; 235:562-567. |
Schmid elaborated on the protocol in an e-mail to AuntMinnie.com. "The MR protocol in our institution preoperatively usually includes sagittal T1- and T2-weighted sequences and an axial T2-weighted sequence," he explained. "In the postoperative setting we often use the same protocol. In case of postoperative suspicion of infection or bleeding, we additionally use gadolinium-enhanced T1-weighted axial and sagittal sequences with/without fat suppression. But we do not perform routinely postoperative MR control examinations if the patient is doing well."
According to the results, all 60 patients had at least one disk extrusion at preoperative MR imaging, as well as neural compromise. Advanced disk degeneration (grades IV and V) occurred more frequently in the control group. No disk degeneration or minor degeneration was seen before initial surgery in 83% of the study group and 50% of the control group.
"The risk of recurrent disk herniation was reduced by a factor of 3.4 for each increase in the grade of disk degeneration," the authors explained. "A normal intervertebral disk (grade II at MR imaging) in an adult has a 6.8-fold increase in the risk of recurrent herniation, as compared with the risk of a disk with advanced degeneration (grade IV)."
The outcome of this study has prompted orthopedic surgeons to inform patients more carefully about the risk of recurrence, Schmid told AuntMinnie.com. The surgeons will refuse to perform diskectomy on a patient with questionable MR findings because of the increased risk of recurrence, but those are very rare and selective cases, he added.
By Shalmali Pal
AuntMinnie.com staff writer
May 10, 2005
Related Reading
MR neurography proves itself in sciatica and beyond, April 15, 2005
Osteopath proselytizes for musculoskeletal US, November 11, 2004
Copyright © 2005 AuntMinnie.com