In a study with important implications for patients in emergency rooms, Italian researchers have shown that contrast extravasation can be readily seen on contrast-enhanced ultrasound. CT confirmed the findings in most of the patients.
"Contrast medium extravasation is a well-known CT and angiography sign of ongoing traumatic or nontraumatic hemorrhage," said Dr. Bianca Cusati at the 2004 RSNA meeting in Chicago. "It is usually considered as a predictor of conservative management failure and need for immediate surgery."
Some experimental studies have shown that contrast-enhanced ultrasound can detect active bleeding, she said. In their study, Cusati, from Santa Maria delle Grazie Hospital in Pozzuoli, Italy, and Dr. Orlando Catalano from the Istituto Nazionale per lo Studio e la Cura dei Tumori, Fondazione G. Pascale (INT) in Naples, examined 153 consecutive patients who underwent emergency contrast-enhanced ultrasound after admission to the hospital's emergency department during 2002 and 2003.
"We report our limited experience in the assessment of the possibility to detect contrast leakage by using contrast-enhancement ultrasound," she said.
The cohort included 83 patients with traumatic injuries and 70 with nontrauma emergencies. Twenty-nine studies were performed in the emergency room, 11 at the patient's bedside, and 113 in the radiology department, Cusati said. Nine patients were considered stable and 144 were unstable.
Scanning began immediately after a 2.4- to 2.8-mL bolus injection of SonoVue (Bracco, Milan, Italy), and lasted from one to four minutes. The exam was performed using contrast-specific mode and contrast-tuned imaging (EsaTune, Esaote, Genoa, Italy) using a continuous-mode low mechanical index technology.
"Active bleeding appears as a round or oval spot of contrast (pooling), or clear jet of opacified blood -- hyperechoic compared to surrounding tissue and isoechoic in comparison with vessels"; the subcontinuous findings were detected immediately after vessel opacification, she said. "After an initial high-powered flash (the extravasation) vanishes, to appear again a few seconds later."
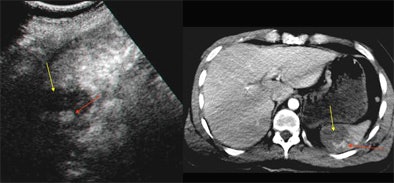 |
| Contrast-enhanced ultrasound (left) and contrast-enhanced CT (right) of the spleen. Oblique sonogram shows a large deep hypoechoic area of splenic laceration (yellow arrow) with internal hyperechogenicity due to contrast medium pooling (red arrow). The CE SSCT shows similar findings, confirming the injured area (yellow arrow) and the contrast leakage (red arrow). All images courtesy of Dr. Bianca Cusati. |
The active bleeding tends to pool independently from any parenchymal or extraparenchymal source, the authors noted in an accompanying abstract. "The bleeding should be differentiated from calcifications, opacified normal vessels, and still-vascularized areas within the parenchyma."
"In this patient with abdominal aortic aneurysm, baseline ultrasound shows the focal interruption of the aneurysm and left-sided resulting hematoma," Cusati said. "Contrast enhancement shows contrast extravasation.... In another image, "the contrast-opacified lumen of the aorta, after contrast extravasation, could be recognized as a hyperechoic jet, splashing through the aortic wall...."
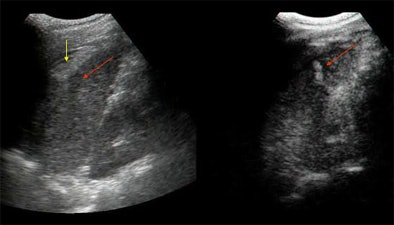 |
| Baseline (left) and contrast-enhanced (right) US scan of the spleen in a trauma patient. A subtle hypoechoic area is recognizable at spleen middle-third level on unenhanced image (red arrow); there is also subcapsular hematoma (yellow arrow). Contrast-enhanced image demonstrates a clear lacerocontusive perfusion defect with a central hyperechoic spot due to active extravasation (arrow). |
The cases included splenic trauma (n = 9), liver trauma (n = 3), renal trauma (n = 1), ruptured abdominal aortic aneurysm (AAA) (n = 4), surgical repair for AAA (n = 1), ruptured splenic angiosarcoma (n = 1), and splenectomy (n = 1).
Contrast-enhanced US detected contrast extravasation in 20/133 (13%) cases overall, with a positive predictive value of 100% based on the 9/20 cases for which confirmatory CT was available. Ultrasound's negative predictive value was also 100% based on the 57/133 negative cases for which confirmatory CT was available. Clinical correlation was also available to confirm the ultrasound results in 13/83 (16%) trauma cases and 7/70 (10%) nontrauma cases.
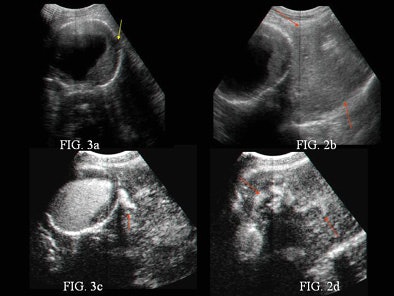 |
| Baseline sonogram (a-b) and contrast-enhanced US scan (c-d) of an abdominal aortic aneurysm. The baseline sonogram shows focal interruption of aneurysm (small hypoechoic focus adjacent to the aneurysm, yellow arrow) and left-sided retroperitoneal hematoma (red arrows). |
"Contrast-enhanced ultrasound should not be intended as a substitute for CT, but as a selective possibility to boost ultrasound's role in acute patients (for) initial screening," Cusati concluded. "This opportunity may be particularly helpful in life-threatening conditions, when ultrasound is performed as the initial, quick, and transportable imaging technique. Our study shows for the first time how contrast-enhanced sonography in the assessment of abdominal emergencies can detect active bleeding."
The technique has interesting possibilities for trauma-patient management, perhaps in combination with the FAST or modified FAST technique that is coming into common use in the U.S., one audience member said.
Another asked how many organs could be checked for active bleeding in the few minutes before the contrast enhancement washout. There is time to examine all of the abdominal organs, Cusati said. The oral contrast agent is very easy to use, and can be prepared in about five seconds, she added.
A radiologist from the University of California, San Diego, said the group's results were impressive, but cautioned that "it takes a lot of operator expertise to do the contrast ultrasound study well. If you don't have a specific organ to look at, it would be difficult to determine where there is active extravasation," she said.
Few studies on extravasation
Another study presented at the RSNA meeting, by Rebecca Joy from the Royal London NHS Trust in the U.K., examined the incidence of contrast extravasation during CT exams, both in radiology literature and from the group's own clinical experience over a year with the management of contrast extravasation injuries.
A literature search yielded only one study that assessed the incidence of contrast extravasation; the results showed extravasation in 0.9% of the CT scans, Joy and colleagues noted in their abstract.
The referenced study, by Dr. Michael Federle et al from the University of Pittsburgh Medical Center, found that none of the 48/928 patients with demonstrated contrast extravasation needed surgical intervention or suffered permanent long-term effects. The incidence of contrast extravasation did increase with the use of power injectors during CT exams, Federle and colleagues concluded, but the group found no correlation between injection rate and the incidence of extravasation (Radiology, March 1998, Vol. 206:3, pp. 637-640).
"Our experience was of a lower incidence (compared to the Federle study), but of varying management responses to the problem," Joy and colleagues wrote in their RSNA abstract. "This led to the formulation of Trust guidelines to deal with the problems that can potentially result from extravasation of intravenous contrast."
By Eric Barnes
AuntMinnie.com staff writer
January 25, 2005
Related Reading
Ultrasound turns in middling results in blunt abdominal trauma, December , 15, 2004
Overexposed? CT in the emergency room, October 21, 2004
Experience beats speed in emergency FAST training, June 2, 2004
Contrast ultrasound shows potential for prostate cancer detection, October 24, 2004
Contrast-enhanced ultrasound not just for cardiac applications, May 14, 2003
Copyright © 2005 AuntMinnie.com




















