Constrictive Pericarditis:
Clinical:
Acute pericarditis is usually idiopathic (80-85% of cases) and
these
care are generallly presumed to be viral in origin- typically
coxsackie,
parvovirus B19, herpes virus 6, echovirus, and HIV [4,5]. Less
common
causes include uremia, certain drugs (hydralazine, procainamide),
hypothyroidism, TB, autoimmune disease, and neoplastic pericardial
infiltration [4,5]. It can
also be seen in about 10% of patients following transmural
myocardial
infarction (this is called Dressler
syndrome when the onset is delayed and it is related to an
autoimmune
origin) [4,5]. Iatrogenic causes include post radiation therapy
for
breast cancer or mediastinal tumors, follwoing cardiac surgery or
percutaneous interventions, pacemaker insertions, or catheter
ablations
[5]. Acute pericarditis is often accompanied by some degree of
myocarditis (myopericarditis) [5].
With acute pericarditis there is
usually only minimal pericardial thickening [4]. Late gadolinium
enhancement may be seen and characteristically localizes along the
pericardium or epicardial layer [4]. A pericardial effusion, if
present, is usually small [4]. Most cases of acute pericarditis
are
benign and most patients respond favorably to treatment with
nonsteroidal anti-inflammatory drugs [5]. The condition may
progress to
chronic sclerosing pericarditis which is characterized by
fibroblasts
and collagen deposition that leads to a stiff pericardium
(constrictive
pericarditis) [5]. The risk of constrictive pericarditis after
acute
pericarditis is very low in viral or idiopathic pericarditis (less
than
0.5%), but is relatively frequent in purulent and tuberculous
pericarditis [5]. Post radiation and post operative constrictive
pericarditis have become some of the most frequent causes of the
disorder [5].
Constrictive pericarditis results in impaired diastolic filling
of
the heart due to
fibrosis and thickening of the pericardium- pressures between the
atria
and ventricles
equilibrate. Patients present with symptoms similar to those of
CHF-
dyspnea, leg
swelling, pedal edema, hepatomegaly, and jugular venous
distention. An
associated finding
on physical exam is "Kussmaul's sign"- a paradoxical elevation of
jugular venous
pressure that occurs during inspiration.
Prior to antibiotics, TB was the most common
cause of constrictive pericarditis. Tuberculous pericarditis
occurs in
1% of
cases of TB [2]. The pericardial involvement is typically due to
extranodal
extension of lymphadenitis [2]. A constrictive pericarditis occurs
in
about 10%
of patients with tuberculous pericarditis [2]. Presently, an
antecedent
clinically inapparent viral
pericarditis is probably the most common etiology for constrictive
pericarditis. Other causes include prior mediastinal
XRT, cardiac surgery (0.2% of post-sternotomy patients), uremia,
rheumatic fever, and
collagen vascular disease. About 50% of patients demonstrate
pericardial calcification,
especially if the pericarditis was the result of a viral
(Coxsackievirus) or Tuberculosis
infection.
Clinically, it is important to distinguish constrictive
pericarditis from
restrictive cardiomyopathy- each of which have similar clinical
presentations and
hemodynamic alterations at catheterization. Pericardial stripping
(pericardiectomy) may
result in a dramatic
improvement in symptomatology. Long term survival after
pericardiectomy
is related to the underlying cause of the condition and survival
in
post radiaiton constrictive pericarditis, survival is poor [5].
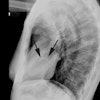
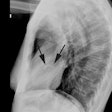
X-ray:
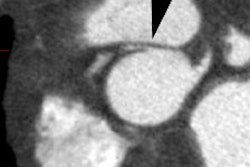
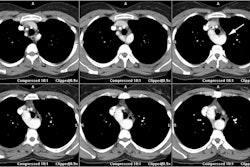
Both CT and MR effectively demonstrate pericardial thickening.
On CT, the normal pericardium measures between 1-2 mm, and a
pericardial thickness of more than 4 mm is generally regarded as
abnormal, and more than 5-6 mm is highly specific for constriction
[5].
However, normal pericardial thickness (2 mm or less) can be seen
in 14-20% of patients with constrictive pericarditis (and this may
indicate later stage disease) [5,6]. Also- up to 25% of patients
without constriction can have a pericardial thickness of 4mm
or more [6]. In patients with pericardial constriction, the IVC
will enlarge [6]. An IVC cross-sectional area ≥ 7.5 cm2 and an
IVC-to-aortic area ratio ≥ 1.6 (sensitivity 95%, specificity 76%)
can aid in the identification/confirmation of pericardial
constriction [6]. The phase of the respiratory cycle affects the
size of the IVC [6]. A dilated IVC with absence of collapse by
more than 50% in inspiration is considered a marker of increased
RA pressures [6]. Because CT imaging is performed at
end-inspiration, IVC measurements are a representation of RA
pressures [6].
Pericardial calcifications are another important sign of constrictive pericarditis (although pericardial calcificaiton is less common than in the past and is now seen in 27-28% of patients) [5]. Diffuse enhancement of the pericardium can also be seen on post contrast imaging [5]. Pericardial calcification is best appreciated on CT, but MR can provide more hemodynamic information. Pericardial calcification can be shaggy (more common and typically within the atrioventricular groove) or egg-shell (less common- spares portions of the left atrium not covered by pericardium).
On MR, the normal pericardium appears as a curvilinear line of
low
signal intensity
situated between the high signal intensity of the pericardial and
epicardial fat. It
normally measures 1 to 2 mm in thickness [5] - a width of up to 4
mm is
not
necessarily
pathologic [3]. Small quantities of pericardial fluid may be seen
normally in the superior
pericardial recess (posterior to the ascending aorta). A
pericardial
thickness of greater
than 4 mm is considered evidence of constrictive pericarditis in
the
appropriate clinical
setting. Caution must be exercised in patients with a history of
cardiac surgery or
post-pericardiotomy syndrome as they may have significant
pericardial
thickening in the
absence of clinical symptoms. Unfortunately, the absence of
pericardial
thickening does
not exclude constrictive pericarditis [4]. Cine MR can be used to
evaluate for constrictive pericarditis in cases of normal
myocardial
wall thickness [5]. Findings include narrow tubular shaped
ventricles,
a
sigmoid shaped septum,
dilatation of the right atrium, SVC, IVC, and hepatic veins, and
abnormal ventricular
movement against the pericardium. Phase contrast MR imaging of the
tricuspid valve inflow will show a restricitve filling pattern of
enhanced early filling and decreased or absent late filling,
depending
on the degree of pericardial constriction and increased filling
pressures [5]. Also- flow in the IVC shows restrictive physiology
with
diminished or absent forward, or even reverse, systolic flow,
increased
early diastolic forward flow, and late reversed flow [5].
Constrictive
pericarditis, in contrast to restrictive cardiomyopathy, is
typically
characterized by a strong respiratory-related variation in cardiac
filling (ie: enhanced RV filling on inspiration and enhanced LV
filling
on expiration [5].
REFERENCES:
(1) Magn Reson Imaging Clin N Am 1996; May 4(2): 237-251
(2) Radiographics 2001; Kim HY, et al. Thoracic sequelae and complications of tuberculosis. 21: 839-860
(3) AJR 2002; Kovanlikaya A, et al. Characterizing chronic
pericarditis using
steady-state free-precession cine MR imaging. 179: 475-476
(4) AJR 2011; Hoey ETD, et al. Cardiovascular MRI for assessment
of
infectious and inflammatory conditions of the heart. 197: 103-112
(5) Radiology 2013; Bogaert J, Francone M. Pericardial disease:
value of CT and MR imaging. 267: 340-356
(6) J Cardiovasc Comput Tomogr 2014; Hammeman K, et al. Cardiovascular CT in the diagnosis of pericardial constriction: predictive value of inferior vena cava cross-sectional area. 8: 149-157