AuntMinnie.com presents Part II of a four-part white paper on pediatric imaging tips and techniques by Douglas Clark, R.T. (R) (CT).
You've brought a child and his parents to the x-ray suite. Now what happens? Do the parents go inside with you or do they wait in the hall? Is the child going to cooperate better with them in the room and make everyone's lives easier?
Unless your department has a policy in place regarding parents in the procedure room, this really works out to be a case-by-case decision. Children, regardless of age or maturity level, act a little differently when you get them in the room. Is it the white-coat syndrome that makes them freeze? Are they all over the place and hard to keep still? Do they understand what you're telling them? Just like adults, our job is easier if you explain first and attempt to ensure their cooperation.
What can we do to make a child more at ease? Having a parent there sometimes works. Let your patient touch the camera or turn the light on. How about having them hold the cassette while you move the tube, or put the ID card in the flasher? Giving your patients some modicum of control in the situation sometimes makes them more open. The promise of stickers or other treats after the exam quiets kids down a lot, too.
How do we get the child to hold still for the procedure? There’s always tape (I should buy stock in 3M) as a gentle reminder to keep the extremity still. Sandbags or pillows work on occasion. Having the parents stay in the room and hold the child in position (remember to give them a lead apron) is an alternative, especially if you're working alone.
How about that old torture device we all used at one time or another, the Pigg-O-Stat? It was scarier for the parents than for the child, but it works great and immobilizes the patient.
Remember to shield your patients and anyone else in the room if doing CT; an apron goes both under and over the patient.
No matter what method we use to ensure cooperation, praise goes a long way at the end of the exam to ensure cooperation in the future. Don't be afraid to tell them they did a good job.
Imaging tips
Although the exams we do might be the same as those conducted on adults, our techniques certainly differ with these little people. In most cases, try to keep your kV below 70. Because we can go non-grid with most things, we’re able to drop the mAs significantly too.
Talk to your radiologist or supervisor about pediatric protocols and department standard operating procedures (SOPs) for children. Most will limit the number of views or regions that we cover.
How about image evaluation? It says in the rules and regulations of the American Registry of Radiologic Technologists (ARRT) that we "do not interpret studies." We are, however, allowed to evaluate the images technical quality and make observations.
For instance, you have a young man with what appears to be a broken forearm on plain film. Your hospital's policy is that you image the patient and let them sit in the waiting room, telling them that the radiologist will call their doctor. Meanwhile, the radiologist is doing a barium enema and looking at an ultrasound while trying to return another call.
You leave the films on the desk and when he picks them up an hour or so later, he asks why you hadn’t brought them to his attention. Most radiologists will appreciate the heads up, such as: "Something looks funny about his film. Can you look at it before I sit this kid back outside?”
We also want to evaluate the film for image quality. Can you see all the anatomy that you’re supposed to? Is the collimation appropriate? Is the film too dark or too light? The comment, "That's what they make hot lights for" definitely does not fly with pediatrics.
Many years ago a preceptor taught me a valuable lesson: If you have to look at it more than once or ask someone else’s opinion, then you need to repeat it, period.
Case studies
Let’s take a few minutes and look at some challenging cases and radiographs for technical, as well as pathological, findings.
 |
| Figure 1 |
 |
| Figure 2 |
In figure 1 we have an attempted AP view of the elbow in a 10-year-old male. Because the child was unable to fully extend his arm, his body was partially oblique to the affected side, and the arm was extended as far as possible.
Upon completion of the lateral film (figure 2), which was done with the film tucked between the child's arm and his body and shot cross-table in a wheelchair, it is evident why the arm is in a fixed position. Note the subluxation of the humeral condyles from the olecranon process (arrow).
Let’s look at another challenging, but common, orthopedic case: forearm fracture.
 |
| Figure 3 |
 |
| Figure 4 |
In figure 3 there is an obvious midshaft fracture of the forearm on the AP view. The film was shot with the forearm in a position of comfort on the child’s lap. On the attempted lateral, figure 4, we see that because of the deformity, it is not a true lateral. It, again, was shot cross-table with the film braced between the child and his forearm.
How about chest x-rays? Probably one of the most common things we see ordered in any department. What’s good and bad?
First of all, we need to see 8-10 pairs of ribs on a good inspiratory chest. It cannot be over-penetrated or rotated. Look at the position of the SC joints and scapula.
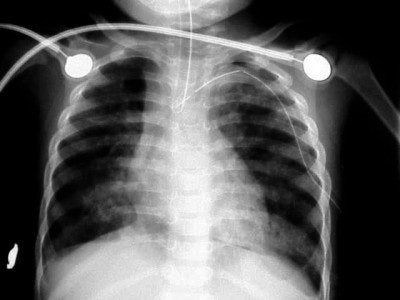
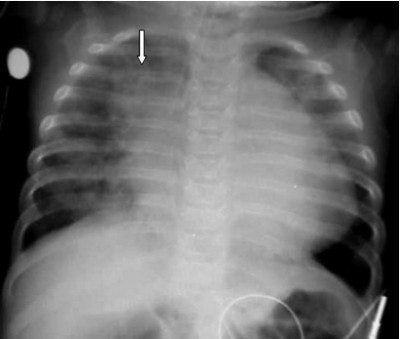 |
| Figure 5 |
In figure 5 we have the chest x-ray of a six-month-old infant with cough, fever, and shortness of breath (SOB). Nine pairs of ribs are visible, the arms are raised above the child’s head, and there is no evidence of rotation. Pathologically, he has right upper lobe aspiration pneumonia (arrow). The darker area in the left lung base was diagnosed as a pneumothorax, cardiomegaly; something is displacing the ET tube to the right. A chest CT was recommended for further evaluation.
Now let’s try something a bit more diagnostic. This is a case of iatrogenic injury, an injury caused by the treatment of a physician.
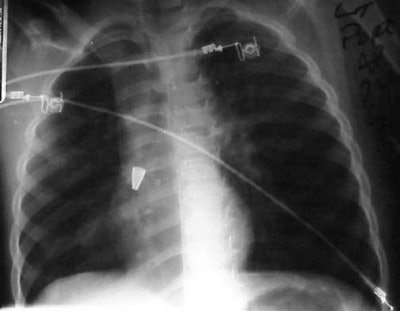
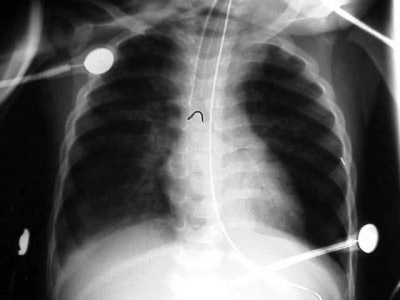 |
| Figure 6 |
 |
| Figure 7 |
 |
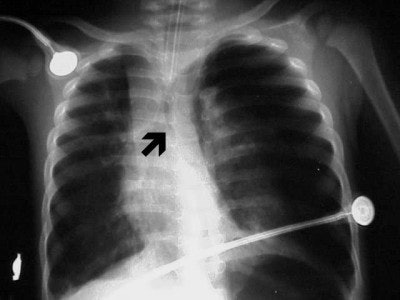
| Figure 8 |
In figure 6 we have a 24-month-old who has been intubated, with a diagnosis of RSV. The film is slightly overpenetrated as we cannot clearly make out lung markings, but we can see the bronchial air shadow and the tip of the ETT (marker arrow), which is right at the carina (the bifurcation of the right and left mainstem bronchus). Doctors attempted to re-position the ETT and the left lung is ruptured causing a tension pneumothorax (arrow, figure 7).
In figure 8, the radiographic technique has been adjusted to show lung markings after the placement of a chest tube on the left. The chest tube, however, appears to be abutting the ETT, and notice the air shadow extending around the pericardium and along the diaphragm, consistent with the diagnoses of pneumomediastinum.
In some cases of non-accidental trauma (formerly called child abuse) we see infants with skull fractures. These eggshell fractures (figures 9 and 10) are consistent with the child’s being held by his ankles and swung against an inanimate object, in this case, a coffee table.
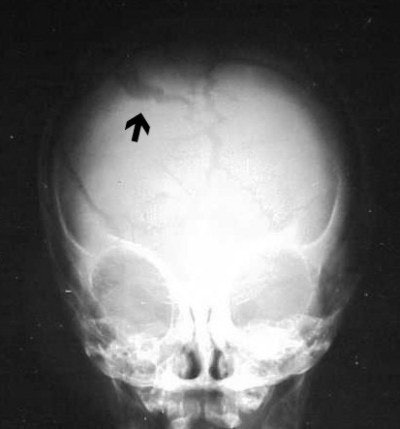 |
| Figure 9 |
 |
| Figure 10 |
How about the infamous ingested object, be it radio-opaque or radiolucent? First of all, try to get the real story. Realize the importance of quality images, without rotation, in trying to gauge placement of the foreign object. If it is lodged in the bronchus, the child might have to go to surgery.
 |
| Figure 11 |
In figure 11 we have a KUB image of a 24-month-old who has swallowed a marble that is in the process of passing through his GI tract.
 |
| Figure 12 |
Figure 12 shows an eight-year-old girl who has swallowed her diary key. I sat her on my knee and asked her what would happen the next time she had to write in the diary. Her quizzical expression and that inevitable look of realization were priceless.
Figure 13 is an incidental finding in a five-year-old boy on his pre-op chest x-ray. This is the tip of an old ballpoint pen. Doctors think he swallowed it some time ago, and on bronchoscopy they found that a pus pocket formed around it, just off the right mainstem bronchus. They were able to remove the pocket and the cap and the child went on to have his appendectomy.
 |
| Figure 13 |
As a final thought on foreign bodies (FB), what happens if your FB is radiolucent? Figure 14, below, is a chest radiograph of a child who has allegedly swallowed a peanut. Is there anything apparent? What other views could, or should, we take to demonstrate the possible foreign body?
 |
| Figure 14 |
We see a good inspiratory chest x-ray, a good radiographic technique, and no obvious radio-opaque FB.
However, a chest x-ray done on expiration, figure 15, below, shows hyperinflation or air trapping of the right lung field, consistent with ball-valve effect or obstruction at the level of the right mainstem bronchus.
 |
| Figure 15 |
Bronchoscopy confirmed the presence of a peanut at the level of the bronchial bifurcation on the right, and the child underwent an uncomplicated "peanut-ectomy."
By Douglas Clark
AuntMinnnie.com contributing writer
April 26, 2004
Join us on May 7 for Part III: Imaging the pediatric patient: CT contrast and sedation.
Clark is a staff CT technologist with University Health System in San Antonio, TX, and has been a radiologic technologist since 1990.
Related Reading
Part I: Imaging the pediatric patient: Beyond the smiles and stickers, April 22, 2004
Misread scans often lead to osteoporosis diagnosis in children, March 22, 2004
PET/CT brings added value to pediatric oncology, February 27, 2004
Ultrasound, CT, or MRI best for pediatric foot toothpick puncture injuries, February 25, 2004
Bladder shape affects pediatric ultrasound bladder-volume estimates, August 29, 2003
Copyright © 2004 Douglas Clark