A study of older Americans has found that better access to screening colonoscopy since 1998 has led to the detection of more right-sided and early-stage colorectal cancers. The findings, reported in the December 20 issue of the Journal of the American Medical Association, suggest that reimbursement for colorectal cancer screening may significantly, and perhaps cost-effectively, reduce mortality from the disease.
Still, limited screening resources mean that universal colorectal cancer screening will remain an impractical goal, according to an editorial accompanying the study. The editorial recommends that ways of identifying the highest-risk elderly patients should be found to direct limited screening resources to the population most likely to benefit from it. Neither paper suggests the wider use of virtual colonoscopy, a whole-colon exam that many radiologists consider an essential part of the solution to limited screening capacity in the face of a fast-growing U.S. population of older, screening-age individuals.
Regular screening is the most effective way to find colorectal cancer while it is still curable, though widespread screening has consistently lagged behind recommended levels, the study authors note.
In 2000 the National Health Interview Survey found that 42.5% of respondents 50 years of age and older were up-to-date with colon cancer screening with any of the recommended methods; among persons 65 years of age and older, 48.7% were up-to-date, they wrote.
"There are several important barriers to colon cancer screening including patient and physician awareness, preferences, and access to care," noted lead investigator Dr. Gary Gross and colleagues from the Yale University School of Medicine in New Haven, CT. "Several studies have suggested that the lack of insurance coverage may be one of the most important barriers to colon cancer screening (JAMA, December 20, 2006, Vol. 296:23, pp. 2815-2822).
The researchers examined the Surveillance, Epidemiology and End Results (SEER) Medicare-linked database for patients 67 years and older who were diagnosed with colorectal cancer in the 14 years since Medicare-paid screening was implemented in the U.S. in several stages.
Prior to 1998, Medicare beneficiaries were required to pay for all colorectal cancer screening exams out-of-pocket, including fecal occult blood testing, barium enema, and sigmoidoscopy. After the U.S. Congress passed the Balanced Budget Act of 1997, Medicare began paying for the tests beginning January 1, 1998.
"Our objective was to assess whether there was an independent relation between the reimbursement policies and patterns of care with regard to both screening and diagnosis of colorectal cancer in screening beneficiaries," the authors explained.
The SEER population studied were 67 years and older and had a primary diagnosis of colon cancer during1992-2002, in addition to a group of Medicare beneficiaries who resided in SEER areas but were not diagnosed with colon cancer.
"First, to ascertain if the Medicare policies were associated with an increased use of colonoscopy, we identified a cohort of Medicare beneficiaries without cancer who lived in one of the ... (SEER) areas during the study period," they wrote. "We then compared changes in the rate of colonoscopy with that of flexible sigmoidoscopy," and assumed that changes during the study period were related to screening, they explained.
Trends in colonoscopy and sigmoidoscopy billing for Medicare beneficiaries without cancer were assessed using multivariate Poisson regression. Patients with cancer were categorized by stage (stage I versus all other stages) and tumor localization. Time was categorized as period 1 (no screening coverage 1992-1997), period 2 (limited coverage January 1998-June 2001), and period 3 (universal coverage July 2001-December 2002).
"Multivariate logistic regression (outcome = early stage) was used to assess temporal trends in stage at diagnosis; an interaction term between tumor site and time was included," the team wrote.
First, among Medicare beneficiaries who did not have cancer, the use of colonoscopy increased during the study period. The use of colonoscopy increased from an average of 285 out of 100,000 per quarter in period 1 to 889 and 1,919 in periods 2 (p < 0.001) and 3 (p < 0.001), respectively, for each pair-wise comparison, the group reported.
"During the study period, 44,924 eligible patients were diagnosed with colorectal cancer," they wrote. "The proportion of patients diagnosed at an early stage increased from 22.5% in period 1 to 25.5% in period 2 and 26.3% in period 3 (p < 0.001) for each pair-wise comparison."
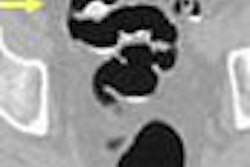
Moreover, the researchers found a strong association between the changes in Medicare coverage and early stage at diagnosis for patients with proximal colonic lesions (adjusted relative risk period 2 versus 1, 1.19; 95% CI, 1.13-1.26; adjusted relative risk period 3 versus 2, 1.10; 95% CI, 1.02-1.17).
However, only a weak association was seen between increased coverage and distal colorectal lesions (adjusted relative risk period 2 versus 1, 1.07; 95% confidence interval, 1.01-1.13; adjusted relative risk period 3 versus 2, 0.97; 95% CI, 0.90-1.05).
Among these patients, there was a statistically significant increase in the probability of early stage at diagnosis from 30.5% in period 1 to 33.2% in period 2; however, the proportion of patients diagnosed at early stage in period 3 did not differ significantly from the period 1 results, they explained.
And although the proportion of fee-for-service colorectal cancer patients diagnosed at an early stage increased in each successive time period, there was no such increase among HMO patients, whose access to screening presumably did not change as dramatically as that of fee-for-service patients with enactment of the new policy.
"We found that the proportion of older colon cancer patients who were diagnosed with early-stage disease increased significantly after the initiation of new Medicare screening reimbursement policies," Gross and his co-authors wrote. "These findings were robust, in that they were unchanged even after accounting for important patients and geographic factors."
The improvements were largely confined to proximal lesions, and patients were only slightly more likely to present with early-stage distal disease after broader coverage was enacted.
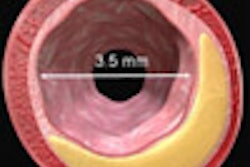
"The selective effect of the coverage change on proximal colon lesions suggests that whole-colon screening modalities such as colonoscopy may have played a pivotal role," they wrote. "This hypothesis is strongly supported by our finding that there was an increase in colonoscopy usage following each of the reimbursement changes, whereas sigmoidoscopy use actually decreased dramatically after the second policy change."
As for limitations, it is difficult to differentiate between diagnostic and screening procedures. However, colonoscopies increased nearly fivefold during the study, while it is unlikely that symptomatic presentations, or the approach to evaluating such presentations, changed dramatically during the study period. Therefore, the increase probably represented an increase in screening colonoscopies, the authors wrote.
"Given that there are approximately 60,000 cases of colorectal cancer diagnosed annually in the United States, even a 4% increase in the percentage of patients whose cancer is diagnosed at an early stage can have a substantial impact on a population level," they wrote.
In an accompanying editorial, Dr. Arden Morris from the University of Michigan in Ann Arbor commented on the study.
"The findings of Gross et al demonstrate that the change in Medicare policy was effective: a target population received screening at a higher rate and this resulted in an increase in the detection of early stage and right-sided cancers," Morris wrote.
"It remains to be seen if future screening will continue to increase the rates of early identification of colorectal cancer. Given the costs of universal screening, if rates of colonoscopy continue to increase without additional benefit in overall diagnosis of early-stage disease, policy makers, healthcare organizations, and physicians may have to devise a feasible rationing plan for broader colon screening. While increasing access to care and improving compliance with recommended care is an undeniable good, providing screening colonoscopy to all is not realistic."
The onus is on physicians and other primary care clinicians to encourage other effective but less expensive forms of screening, such as fecal occult blood tests with sigmoidoscopy, he continued.
In addition, Morris wrote, screening colonoscopy could be made more effective by targeting subgroups with higher incidence and mortality from colorectal cancer, and those at greatest risk of right-sided or proximal neoplasms that would not be identified by sigmoidoscopy.
"Such a strategy, while difficult, would provide the best opportunity to judiciously maximize access to care without sacrificing outcomes," he wrote.
By Eric Barnes
AuntMinnie.com staff writer
December 19, 2006
Related Reading
Slow colonoscope removal increases odds of spotting lesions, December 14, 2006
Colonoscopy declines at VA: Is limited capacity to blame? November 13, 2006
New data reveal higher efficacy for primary VC screening, October 18, 2006
Gastroenterologist surveys target lesions, VC practice, March 20, 2006
Copyright © 2006 AuntMinnie.com