
The herbal root ginseng can be found in everything from shampoo ("a natural hair tonic") to body lotion ("protection against free radicals") to foot bath salts ("used by Olympic athletes"). Then there are ginseng supplements in the form of pills, powders, or pabulum intended for ingestion. Whether it's the American, Asian, or Siberian variety, ginseng is credited with anti-aging and anti-stress properties, as well as being an aphrodisiac.
But too much ginseng can be a bad thing. A 39-year-old woman in Ankara, Turkey, found this out when she presented at the Ankara Numune Training and Research Hospital with prolonged, excessive uterine bleeding and heart palpitations. She was ultimately diagnosed with menometrorrhagia and tachyarrhythmia by the hospital doctors.
The culprits, according to her doctors, were the oral Korean white ginseng capsules she was taking daily, as well as the skin care products (cream, mask, and toner) that also contained Korean red ginseng. An endometrial biopsy revealed "a disordered proliferative pattern consistent with the patient's phase of menstrual cycle." Her ECG showed sinus tachycardia (106 beats/min), and the patient was advised to stop using oral and topical ginseng (Journal of Women's Health, September 2004, Vol. 13:7, pp. 830-833).
At one month follow-up, her ECG was normal, her menometrorrhagia had stopped, and it did not recur for the next six months. Dr. Ayla Kabalak and colleagues suggested that the ginseng competes with estrogen-binding sites and has an estrogen-like effect on the vaginal epithelium.
Kabalak told AuntMinnie.com that the patient underwent transvaginal sonography, which showed minimal endometrial thickening. In general, ultrasound is the modality of choice for finding the underlying causes of menometrorrhagia. Ginseng overdose is a unique reason; more common diagnoses include anatomic pelvic lesions, ovarian cyst, ovarian neoplasm, endometrial lesions, polyps, or carcinoma. Over the last decade, several studies have reiterated the value of ultrasound in these patients.
US versus pelvis exam
Ten years ago, a paper by Dr. Melvin Dodson, Ph.D., touted the superiority of transvaginal ultrasound (TV-US) for diagnosing the etiology of menometrorrhagia.
In his study, Dodson found that "TV-US was about 3.5 times more sensitive in detecting anatomic pelvic changes associated with menometrorrhagia than was pelvic examination.... US can also be of value in confirming some diagnoses that are generally made clinically by exclusion, such as breakthrough bleeding from oral contraceptive use and dysfunctional uterine bleeding (DUB)" (Journal of Reproductive Medicine, May 1994, Vol. 39:5, pp. 362-372).
For this study, 45 women who complained of abnormal vaginal bleeding underwent sonography with a 5-MHz transvaginal probe. Ultrasound revealed anatomic findings in 31% of the patients versus 9% found with clinical evaluation only. Among those patients who had breakthrough bleeding with contraceptive use, 33% had anatomic findings on ultrasound. Sonography was also helpful for differentiating between anovulatory and ovulatory DUB, diagnosing polycystic ovary disease, and predicting hormonal and histologic endometrial status, Dodson wrote.
"Based on TV-US findings ... a more refined diagnosis of the etiology of menometrorrhagia, such as a small ovarian cyst or other anatomic pelvic changes or pathology, was possible," he concluded.
TV-US and adenomyosis
Another possible cause for menometrorrhagia is adenomyosis. Like Dodson, a group from Paris also found that transvaginal sonography aided in the detection of this gynecological disorder. However, they also found that the modality had some limitations.
In accordance with previous studies, Dr. Marc Bazot and colleagues from Hôpital Tenon reported that "a higher prevalence of adenomyosis was found in women who had menometrorrhagia but were free of endometrial disease and leiomyomata" (Ultrasound in Obstetrics and Gynecology, December 2002, Vol. 20:6, pp.605-611).
For their assessment of the accuracy of transabdominal sonography versus transvaginal sonography, they enrolled 129 women scheduled for hysterectomy. Pelvis transabdominal sonography (TAS) was performed using a wideband 2-4 MHz transducer while transvaginal sonography (TVS) was done with a wideband 5-9 MHz transducer. Color Doppler was used to distinguish between a myometrial cyst and a vascular component, or between potential leiomyoma and focal adenomyosis, they explained.
The women were subsequently divided into two groups. Group 1 (23 of 129) consisted of women with recurrent menometrorrhagia but no evidence of leiomyomata and endometrial disease based on TAS. All other patients made up group 2 (106 of 209).
The images were interpreted in real-time by two investigators who noted such features as uterine borders, size, myometrial echotexture, and presence of associated abnormalities. According to the histopathologic findings, the overall prevalence of adenomyosis was 36.4%. Group 1 had 12 women diagnosed with adenomyosis versus nine in Group 2.
In Group 1, TAS yielded a diagnosis of adenomyosis in 12 out of 21 women with one false-positive. TVS yielded the same diagnosis in 17 out of 21 with no false-positives. In Group 2, two women were diagnosed with adenomyosis, and there were three false-positive results based on TAS. TVS revealed adenomyosis in a dozen women with two false-positives.
In Group 1, the sensitivity of TAS was 57.1%, the specificity was 50%, the accuracy was 56.5%, and the positive predictive value (PPV) was 92.3%. In Group 2, the sensitivity of TAS was 7.6%, the specificity was 96.2%, the accuracy was 74.5%, and the PPV was 40%.
In comparison, TVS turned in the following results. For Group 1, the sensitivity was 80.9%, the accuracy was 82.6%, and both the specificity and PPV were 100%. In Group 2, the sensitivity of TVS was 38.4%, the specificity was 97.5%, and the accuracy and PPV came in at 83%.
Combining TAS and TVS increased the diagnostic accuracy in Group 1, but not in Group 2 (91.3% versus 83%), the authors reported. The most specific criterion for adenomyosis was the presence of myometrial cysts.
"TVS has substantially improved the sonographic diagnosis of adenomyosis, especially in women without myomata," they wrote. However, "in patients with an enlarged uterus, the accuracy of TVS was poor in our study (and) the accuracy of TVS was lower in patients with associated disorders."
In these patients, Bazot's group recommended using TAS and TVS for adenomyosis, stressing that the accuracy of these techniques depends on patient characteristics, as well as the sonographic criteria used.
Endometrial abnormalities
One step beyond the transvaginal scan is saline hysterosonography, also known as sonohysterography. Either way, the goal is the find menometrorrhagia's root causes, such as endometrial polyps.
Ob/gyn specialists at Assiut University in Assiut, Egypt, compared TVS and vaginal sonohysterography (SHG) in 106 patients suffering from abnormal uterine bleeding. TVS was performed with a vaginal 5-MHz probe. Polyps were defined as "well-delineated hyperechoic thickening of the endometrium, or when there was diffuse endometrial thickening with hypoechoic lesion," (Acta Obstetrics and Gynecology Scandinavia, January 2000, Vol. 79:1, pp.60-64).
SHG was performed by an investigator who was unaware of TVS results. The SHG protocol consisted of a vaginal ultrasound scan that was started before saline injection in-utero and continued until the entire uterine cavity was clearly depicted during the liquid's forward flow. Finally, the patients underwent diagnostic hysteroscopy, which included histopathology.
According to the results, TVS found 36 endometrial polyps, while SHG revealed 56. SHG also turned in higher sensitivity than TVS (93.1% versus 93.39%), higher specificity (93.9% versus 75.5%), higher accuracy (93.3% versus 68.8%), and higher PPV (94.6% versus 76.2%).
In addition, SHG showed lower false-positive rates (5.4%) and lower false-negative rates (8%) than TVS (25% and 36.2%, respectively). Another shortfall of TVS is that it often misses polyps, especially when they are in a cervical or corneal location, the authors pointed out. TVS also cannot differentiate between endometrial thickening and polyps in many cases.
In comparison, SHG provides a reliable diagnosis, is relatively inexpensive, and can be performed by a well-trained sonographer.
Despite such positive results, saline hysterosonography was, for some time, relegated to playing second fiddle, used to further define abnormalities found on conventional TVS, according to Dr. Sherelle Laifer-Narin and colleagues from the University of California, Los Angeles.
But SHG has a better chance of tuning into abnormalities in a patient with bleeding and normal TVS, they wrote. The group tested this theory in 180 patients who, despite a normal-appearing endometrium, had a history of abnormal vaginal bleeding.
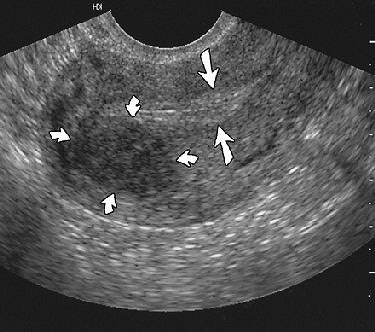 |
| Endometrial polyp in 24-year-old woman. Sagittal sonogram of uterus showing normal-appearing endometrium (straight arrows) measuring 8 mm and posterior uterine leiomyoma (curved arrows). Laifer-Narin S, Ragavendra N, Parmenter EK, Grant EG, "False-Normal Appearance of the Endometrium on Conventional Sonography: Comparison with Saline Hysterosonography," (AJR 2002; 178:129-133). |
Using an intracavity C8-4 transducer, "standard images obtained included a midline sagittal image of the uterus, parasagittal images through the right and left uterine body, and coronal images showing the superior, mid, and inferior portions of the uterus," they explained (American Journal of Roentgenology, January 2002, Vol. 178:1, pp. 129-133).
Of the 180 patients, 114 (63%) showed abnormalities on saline hysterosonography. Polyps were identified in the majority of these patients (54 out of 114), followed by submucosal leiomyomas (38). Sixteen of the 114 showed these abnormalities on saline hysterosonography although their TVS results were normal.
Saline hysterosonography may be more adept at spotting compressed masses that are flattened against the endometrium, they wrote. "Polyps ranged in size from ... 4 mm to 2 cm in greatest diameter. These masses were shorter in the other two dimensions and may ... have been unrecognized on conventional (TVS)."
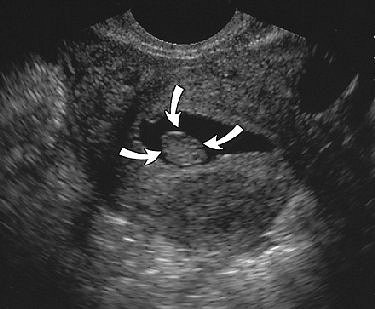 |
| Same patient as above. Sonogram obtained after saline infusion shows homogeneous echogenic mass (arrows) in endometrial cavity, and no submucosal involvement by posterior uterine leiomyoma is present. Laifer-Narin S, Ragavendra N, Parmenter EK, Grant EG, "False-Normal Appearance of the Endometrium on Conventional Sonography: Comparison with Saline Hysterosonography," (AJR 2002; 178:129-133). |
The group did acknowledge some limitations with saline hysterosonography, including a higher cost than TVS and its invasive nature. Furthermore, more than 80% of the patient population in this study was premenopausal. In these women, lesions are difficult to find, regardless of the modality used, they wrote.
Still, endometrial findings may be too subtle and difficult to diagnose on TVS. As a screening procedure, TVS may be insufficient, they wrote. Saline hysterosonography should be seriously considered as a first-line test.
Getting up-to-date
The latest news in gynecologic ultrasound will be presented at the 2004 Radiological Society of North America (RSNA) meeting in Chicago. Dr. Delores Pretorius will demonstrate the practical value of sonohysterography, combined with 3D ultrasound, in routine clinical practice (Education Exhibit 0561EP-OB-e).
A scientific poster will assess the accuracy of 3D ultrasound and contrast-enhanced, transvaginal color Doppler hysterosalpingography for evaluating tubal patency (0616GU-p). Finally, Dr. Edward Lyons will lead a refresher course on the thickened endometrial stripe in postmenopausal women with vaginal bleeding (RC410C).
By Shalmali Pal
AuntMinnie.com staff writer
November 5, 2004
Related Reading
3D ultrasound poised to revolutionize pelvic imaging, September 9, 2004
TVC US on par with SHG for spotting endometrial polyps, August 3, 2004
Sonographic sign reliably excludes ectopic pregnancy, June 22, 2004
Study outlines sonographic findings of pelvic congestion syndrome, April 14, 2004
3-D ultrasound requires understanding of artifacts, July 8, 2002
Copyright © 2004 AuntMinnie.com

















