It was a bold statement to make to a roomful of MRI experts, but Dr. Michael Brandt-Zawadski, the medical director of radiology at Hoag Hospital in Newport Beach, CA, still made it: CT and CT angiography (CTA) are the best overall tests for assessing acute stroke.
"There's a real battle going on between the x-ray-based and magnetic-based techniques as to the daily practice of stroke management," Brandt-Zawadski, said in a talk at the 2007 International Society for Magnetic Resonance in Medicine (ISMRM) meeting in Berlin. "A number of statements have appeared in the literature saying that both MR perfusion-based and CT perfusion-based techniques are useful in differentiating between reversible cerebral infarcts -- manageable in the acute stage -- and those that may be too late in terms of intra-arterial or intravenous salvage."
"MR is a great tool for admiring the pathophysiology of the disease process, but it turns out that CT may be more practical as far as treatment," he added.
Brandt-Zawadski outlined some of the advantages of CT and CTA in this setting: well-tolerated contrast, powerful computer processing (semiautomated reconstructions), information on brain tissue anatomy and pathology, and, of course, speed.
"One big advantage of CT is that in about 20 seconds, you can really image the entire body. So if you're looking for stroke sources, you can image from the heart up to the brain in 20 seconds and get all the information," he said.
But Brandt-Zawadski was not altogether dismissive of MR's value in stroke imaging altogether. Recent advances in stroke imaging have been in MR, he acknowledged, particularly in the area of diffusion-weighted imaging (DWI).
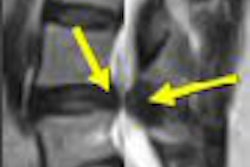
"T2-weighted images don't show us the ischemic brain for some time," he said. "They begin, at approximately 24 hours, to show us the beginning of vasogenic edema. The blood-brain barrier does not break in the first few hours of ischemia. On the other hand, diffusion-weighted images become positive very quickly and over time equalize and, in fact, then reverse ... which acutely shows us the restriction in the cellular space of the water motion."
A multitude of new studies examine the increasing validity of MR in stroke imaging. The technique discussed in two papers is the diffusion-perfusion mismatch model with the goal of devising a "simple and practical means" of pinpointing the ischemic penumbra and identifying patients who are more likely to respond to reperfusion therapy. In the third, DWI results are used to create an outcome prediction model (Stroke, June 2007, Vol. 38:6, pp. 1718-1719).
CDM versus PDM
Perfusion-diffusion mismatch (PDM) is derived by subtracting the lesion volume on DWI from the lesion volume on perfusion-weighted MRI (PWI). Dr. Maarten Landsberg, Ph.D., led the Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution (DEFUSE) investigators in the prospective, multicenter, open-label study of intravenous tPA administered during the three- to six-hour time period after stroke onset. More details on the DEFUSE study methods were published in the Annals of Neurology (November 2006, Vol. 60:5, pp. 508-517).
The 68 patients in this segment of the study had a PDM and clinical-diffusion mismatch (CDM) determined, and agreement between the two models was described as the concordance rate and as Cohen's kappa.
"PDM was defined according to DEFUSE criteria as a PWI lesion volume that is at least 20% and ≥ 10 mL larger than the DWI lesion volume," the group explained. "CDM was defined as a DWI lesion volume < 25 mL and an NIHSS (National Institutes of Health Stroke Scale) ≥ 8" (Stroke, June 2007, Vol. 38:6, pp. 1826-1830).
According to the results, a PDM was present in 54% of the patients and a CDM was present in 62%. Agreement between PDM and CDM models was present in 54% of the patients. The Cohen's kappa was 0.07, which indicated no significant agreement beyond chance between the mismatch models, the authors reported.
The CDM model detected PDM with 65% sensitivity, 42% specificity, a positive predictive value of 57%, and a negative predictive value of 50%. False-positive CDM occurred in patients with small DWI and PWI lesions. False-negative CDM occurred in patients with DWI lesion volumes of more than 25 mL.
For the response to reperfusion analysis, five patients had to be excluded because there were no follow-up PWI results. The authors determined that "mismatch patients selected based on the predefined PDM model were more likely to achieve a favorable clinical response with reperfusion than without reperfusion.... Additional mismatch criteria with potentially discrimination power were identified" based on the parameters set out by the DEFUSE protocol.
"The lack of agreement between the CDM and the PDM models in this study is a direct result of a moderate degree of correlation between PWI lesion volume and NIHSS in our study," they continued. "The relative lack of correlation between PWI and NIHSS may be attributable to several factors, including the possibility that brain tissue that has recently been perfused is not yet functional and the insensitivity of the NIHSS to hypoperfusion in certain areas of the brain."
In a commentary on these DEFUSE results, Dr. Chelsea Kidwell and Dr. Steven Warach, Ph.D., praised the study for showing "the limited role of the clinical-diffusion mismatch model for identifying salvageable brain tissue in the acute stroke setting" (Stroke, June 2007, Vol. 38:6, pp. 1718-1719).
"This is an important reminder that every step away from pathophysiology introduces error and will be a less accurate predictor of tissue outcome and physiological response to intervention" they noted.
DWI for outcome prediction
In a second study, the investigators in the Acute Stroke Accurate Prediction (ASAP) study asked if DWI lesion volume could be used as a prediction model for ischemic stroke. They culled clinical and DWI data from the ASAP database, as well as the Glycine Antagonist in Neuroprotection (GAIN) Americas and GAIN International studies.
"Stroke prediction models ... allow the physician to capture individual information about a patient and project the probability of outcomes to the patient.... We hypothesized that the models with DWI would be valid as determined by an area under the receiver operating characteristic curve (AUC) of ≥ 0.8 for discrimination and a mean absolute error of ≤ 0.4 for calibration when assessed in an external dataset (external validation)," wrote Dr. Karen Johnston and colleagues (Stroke, June 2007, Vol. 38:6, pp. 1820-1825).
Altogether, the researchers gathered data on 648 patients with baseline DWI information. GAIN data were used to develop prediction models using multivariable logistic regression, while ASAP data were used to externally validate the model equations. Clinical predictor variables were age, initial NIHSS score, history of diabetes, prestroke disability, and tissue plasminogen activator (tPA) use. DWI variables were volume, time to DWI scan, and time by DWI interaction. Twelve clinical outcome models were created that predicted either full recovery or disability/death.
For all models with DWI data, age, NIHSS score, and DWI volume consistently contributed to the models (p < 0.05). Five of six full-recovery models with DWI lesion had an AUC ≥ 0.8. The sixth model missed the cutoff with an AUC = 0.799, the authors stated. The man absolute error for each model was ≤ 0.4, with the calibration curves for the models with DWI more closely resembling perfect calibration.
They concluded that "all 12 models had excellent discrimination and calibration" and that DWI lesion volume "significantly increased model explanatory power." However, while DWI did contribute to the prediction of outcome, the magnitude was not significant enough for clinical relevance.
Unlike the previous paper, the authors noted that commonly collected clinical acute ischemic stroke variables, without DWI, may be more useful in an acute stroke setting.
CT scoring versus PDM
Finally, Warach, along with Dr. Steven Messé and colleagues, sought to determine if mismatch between the Alberta Stroke Program Early CT Score (ASPECTS) and NIHSS would correlate with concurrent PDM.
They retrospectively reviewed the results of 143 ischemic stroke patients who underwent multimodal MRI and noncontrast CT at Suburban Hospital in Bethesda, MD. CT images were acquired one of two scanners (Somatom Plus, Siemens Medical Solutions, Malvern, PA; LightSpeed, GE Healthcare of Chalfont St. Giles, U.K.) in the orbitomeatal plane with 5-mm thickness. Based on the 10-point ASPECTS, a score of 10 indicated no early ischemic change. The 1.5-tesla MRI (TwinSpeed XL, GE Healthcare) protocol included DWI, FLAIR, GRE, and PWI imaging. Of these 143 patients, 18% received tPA.
Treatment with tPA is limited to a three-hour time window, the researchers noted. "Unfortunately, the majority of stroke patients are not eligible for treatment because they present at the hospital too late," they stated. "Our study is an important addition to the literature because we included patients who presented well beyond the six-hour time window" (Stroke, May 31, 2007).
The authors found that in this patient cohort head CT and clinical findings could not be used as a way to identify ischemic penumbra as defined by PDM. The median ASPECTS was 10, while the median NIHSS was 4. The median time to scanning completion was 4.5 hour after onset with CT and MRI exams separated by a median of 35 minutes.
"Inter-rater reliability was good for ASPECTS ... with a quadratic-weighted kappa of 0.75. Inter-rater reliability was excellent for determination of MRI mismatch, with a quadratic-weighted kappa of 0.95. Overall, MRI mismatch was present in 58 of 143 (41%) of patients," they wrote. "MRI mismatch was associated with higher NIHSS ... but there was no association with ASPECTS 10 versus < 10 or with any other ASPECTS threshold." In addition, they found no combination of NIHSS and ASPECTS thresholds that were significantly associated with MRI mismatch.
While these results were positive, the group acknowledged that a large number of hospitals do not have the resources to perform emergent MRI, often because the exam is contraindicated in some patients, such as those with pacemakers or hemodynamic compromise. In those settings, head CT, especially with increased time from symptom onset when CT becomes a more sensitive measure of irreversible ischemic injury, would be a reasonable alternative, they stated.
By Shalmali Pal
AuntMinnie.com staff writer
June 14, 2007
Related Reading
Small stroke centers ill-equipped for range of presentations, April 25, 2007
MRI and CT findings comparable in stroke patients, March 9, 2007
MRI should be preferred test for suspected acute stroke, January 26, 2007
MRI profiles predict utility of reperfusion therapy for stroke, November 22, 2006
MRI helps identify ischemic stroke patients likely to benefit from tPA, May 8, 2006
Copyright © 2007 AuntMinnie.com