MIAMI BEACH, FL - Mammography may have its pitfalls when it comes to imaging women’s breasts, but in men, the modality has an impressive sensitivity and specificity, according to two presentations Monday at the American Roentgen Ray Society (ARRS) meeting.
"In 2004, an estimated 1,450 new breast cancer cases will be diagnosed in men. This accounts for less than 1% of all breast cancer cases diagnosed in the U.S," said Dr. Stephanie Patterson from the University of Michigan Health System in Ann Arbor. However, "an appropriate algorithm for the evaluation of male breast problems has not been defined."
Patterson and colleagues looked at the role of mammography and ultrasound in the management of symptomatic men with breast problems.
In a second study, a group from Thomas Jefferson University Hospital in Philadelphia evaluated the diagnostic utility of mammography in men under age 40 with suspected gynecomastia.
Better than ultrasound?
Patterson’s group retrospectively reviewed the records of 163 symptomatic men (ages 29-96) who presented to the breast imaging center over a four-year period. The most common clinical indications for referral were mass/thickening (55% of the cases) and pain/tenderness (30%). The majority of cases (88%) were assigned to BI-RADS categories 1-3. BI-RADS 4 and 5 assessments and any solid sonographic masses were considered suspicious for malignancy, Patterson said.
The mammographers who interpreted the exams were all fellowship-trained in breast imaging; the ultrasound scans were performed by physicians only. Complete follow-up was possible in 84% of the patients, 20% of whom had biopsies.
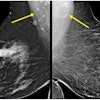
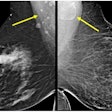
According to the group's results, 4% of the 164 men were diagnosed with primary breast cancer, specifically masses, with spiculated borders, located in the retroareolar area. There were no associated microcalcifications. Five cases were deemed invasive ductal carcinoma and there was one case of ductal carcinoma in situ. In all six of these cases, the mammographic findings were correct. The median tumor size was 2.4 cm in these patients, whose mean age was 64 years.
Fourteen men with suspicious findings turned out to have gynecomastia, lipoma, and other benign cytology, all of which were confirmed with biopsy. All of the patients who had negative mammography results, and did not undergo biopsy, remained cancer-free based on follow-up at one year.
In comparison, ultrasound was performed in 69 out of 164 cases, detecting three solid masses. However, 26% (n=18) of the 69 cases turned out to be false positives.
"This is one of our false-positive cases,” Patterson explained. "The mammogram shows a dense, circumscribed, oval retroareolar mass. On ultrasound, there was a solid mass with some vascular infiltration on Doppler."
The overall sensitivity of mammography in men was 100%, and the specificity was 89%. Out of 20 suspicious mammograms, six proved to be cancer and 14 were benign, yielding a positive predictive value (PPV) of 30%, and a negative predictive value of 100% (NPV). The sensitivity of ultrasound in these instances was 100%, but the specificity was 73%. The PPV was 16% and the NPV was 100%.
"Mammography should be the first imaging study performed (for male breast cancer detection)," Patterson recommended. "Although sensitive, sonography lacks specificity but does provide some complimentary information." Patterson cautioned that her group's study sample was too small to completely rule out the role of sonography in male breast cancer workup.
Session attendee Dr. A. Jill Liebman asked Patterson if compliance was as much of an issue in Ann Arbor as it is at Liebman's New York institutions, where a significant proportion of BI-RADS 4 and 5 male patients were either lost to follow-up or refused a biopsy.
Patterson said compliance rates were high because the patients were referred to imaging by breast surgeons, who continued to treat the patients.
Bypassing biopsy
Gynecomastia occurs more commonly in men than breast cancer and generally affects a younger population, according to Dr. Brian Englander. It's a subareolar density with three patterns of progressive glandular appearance: nodular, dendritic, and diffuse.
This enlargement of the male breast, which can be painless or present as tenderness, is brought on by hormonal imbalances that are either idiopathic, related to puberty, or drug-related (cardiac medicines).
"What I wanted to look at was the role radiology plays in diagnosing gynecomastia and whether more invasive procedures were necessary," Englander said during his talk. At the time of the study, Englander was at Thomas Jefferson; he is now at Pennsylvania Hospital in Philadelphia.
For this retrospective study, 60 men (ages 16-40) underwent diagnostic evaluation over a decade. They underwent both modalities, resulting in reports and images from 60 mammograms and 26 ultrasound exams. The mammograms consisted of mediolateal and craniocaudal views. Out of this patient population, a dozen also had surgical or core biopsy.
Of those 12, 10 with demonstrated gynecomastia had their diagnoses confirmed with biopsy and radiological-pathologic correlation. The remaining two patients, who had masses associated with palpable abnormalities on mammography, were found to have benign breast tumors, lipoma, and pilomatricoma.
Overall, 83.3% of the patients were diagnosed with gynecomastia or normal breast tissue on mammography; 16.7% had benign breast tumors. There were no cases of cancer, Englander said.
Englander's group concluded that men under the age of 40 with a radiologic diagnosis of gynecomastia, and no evidence of a discrete mass, should skip biopsy or other invasive measures. Unlike with female patients, follow-up can be limited to clinical management, Englander said. Performing biopsy on these patients can be costly, and may be an inappropriate use of resources, he added.
Englander said he is planning to fine-tune mammographic technique in these patients. "We're looking at whether chest-wall displacement, similar to what's used in women with implants, will have any value in imaging these patients," he said.
With regard to protocol, a session attendee asked Englander if the exams had been unilateral or bilateral, even when patients’ symptoms were only unilateral. Englander said that bilateral exams were done for the sake of comparison. In answer to another question, Englander said he advocates ultrasound, rather than mammography, in male patients under 16 years of age in order to reduce radiation exposure.
By Shalmali Pal
AuntMinnie.com staff writer
May 3, 2004
Related Reading
Residents leery of careers in breast imaging, December 15, 2003
Increased risk of male breast cancer seen in prostate cancer patients, March 26, 2003
Male breast cancer more common, outcome better among Ashkenazi Jews, April 18, 2002
Copyright © 2004 AuntMinnie.com