VIENNA - When breast computer-aided detection (CAD) software took a second look at mammograms containing a malignancy, it found most of the cancers radiologists had missed until they detected it in a later exam. In some cases, CAD found cancers that weren't detected until three to four years later.
Breast CAD systems have progressed rapidly in recent years, with significant decreases in false-positive rates in newer software iterations.
Some studies report advantages in the detection of cancers with CAD, especially among more inexperienced radiologists, said Dr. Ansgar Malich, Ph.D., from Friedrich-Schiller University's Südharz-Krankenhaus Academic Hospital in Nordhausen, Germany.
Yet the systems' limitations persist stubbornly, particularly the high false-positive rates, he said in a presentation at this week's European Congress of Radiology (ECR). "And there is discussion as to whether CAD use actually produces more recalls and recommended procedures on breast lesions."
The study sought to assess the results of breast CAD software (Second Look, version 6.0, iCAD, Nashua, NH) on mammograms that were positive for cancer but missed by the radiologists until a later breast exam. If these cancers could have been detected earlier with CAD, the researchers surmised, patients might have avoided the delay in diagnosis while their disease continued to progress.
Woulda, coulda, shoulda
A search of the hospital database found 278 such cancer-containing mammograms containing cancers of any size, 97 of which were available in two-view mammograms. For the study, each of these mammograms was examined by two radiologists in consensus.
"These two radiologists knew the cancer-containing images, and they knew where the cancer grew," Malich said. "They had to verify that cancer was visible on the prior images, and they had to rescore the mammograms based on BI-RADS and American College of Radiology (ACR) criteria, and characterize the lesion on the prior mammograms."
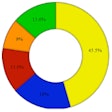
The results were divided into five groups based on the time interval between when the prior mammogram was acquired and when the ultimate detection of cancer was made.
In per-patient results, malignant masses could be seen retrospectively in 53 of the 97 cases, and microcalcifications in 17 of the cases. Thirty of these 53 cases were detected by CAD in one view and four in both views (64%). Eight of the 17 microcalcifications were detected in one view and seven of the 17 in both views (88%).
The detection rate for the malignant masses was 10 of 14 (71%) for the period less than six months after the initial mammogram, four of seven (57%) for less than one year, three of five (60%) for less than 1.5 years, five of seven (71%) for less than two years, three of nine (33%) for less than three years, and nine of 11 (81%) for less than four years. For microcalcifications, the same figures were one of two for the period less than six months, three of four for less than one year, one of one for less than 1.5 years, two of two for less than two years, two of two for less than three years, and six of six for less than four years.
"To be honest, it was a little bit shocking to us that the cancer was in a single case as far as four years prior to radiologic detection with CAD," Malich said.
But what to do with CAD positives?
About half of the initially nondetected cancer-containing mammograms had a mammographically visible lesion that was initially not suspicious according to BI-RADS criteria, and CAD found the majority of these masses and microcalcifications. Yet there is no doubt CAD remains limited, and still produces a high false-positive rate, Malich said.
"But on the other hand, there is a relevant number of structures not being detected by radiologists or not detectable by radiologists that are highlighted by CAD detecting cancer," Malich said. "So why not have a second look at highlighted areas using a reduced false-positive (setting)?"
One audience member wanted to know what Malich would do if CAD highlighted a region that he didn't find suspicious at all. Malich said he would show it to a colleague, and if any doubt remained, the lesion's BI-RADS classification would potentially be upgraded.
On the other hand, CAD results must be taken with a grain of salt. The iCAD software "neither passes the (mammography) screening test nor assists radiologists in a significant manner to pass this test," he noted.
"The problem is that there's an inference that radiologists would behave in a particular way if the tumor was prompted to them," commented Dr. Steve Halligan from St. Mark's Hospital in London. "What we do know is that when radiologists see a correctly highlighted lesion they very often ignore it."
By Eric Barnes
AuntMinnie.com staff writer
March 6, 2006
Related Reading
Mammography CAD: Getting malpractice insurers on board, October 21, 2005
CAD marks: To save or not to save? September 1, 2005
CARS panel discusses the future of CAD, June 28, 2005
CAD may unmask unsuspected cancers in diagnostic mammo, October 27, 2004
New software version cuts false-positives in breast CAD, March 10, 2004
Copyright © 2006 AuntMinnie.com