According to a growing number of breast imaging specialists, the use of computer-aided detection (CAD) in screening mammography is clinically viable, doesn’t produce a mountain of false-positive findings, and boosts radiologists’ ability to detect early-stage cancers.
Because of these favorable reports, the technology, which uses a computer-based algorithm to detect suspicious lesions in digital images, is gaining support as a powerful complement to screening mammography.
"CAD is an extra set of eyes," said Dr. Michael A. Cohen, medical director of the Memorial Sloan-Kettering Cancer Center’s Guttman Diagnostic Center in New York City.
Since August, Cohen and colleagues have used the ImageChecker CAD system (R2 Technology, Los Altos, CA) at the Breast Exam Center of Harlem, an outreach center that provides free screening to women in the neighborhood. The facility screens about 30 women a day.
Each mammogram is first read in the conventional manner by a radiologist. The film is digitized and analyzed with the CAD algorithm, which labels calcifications and masses with icons. The radiologist then compares his or her assessment with whatever the CAD system has highlighted, much like using a spell check tool in a word-processing document.
"It may pick up a cancer that you’ve already seen, and it may also direct you to calcium that you entirely overlooked," Cohen said. "We’ve called several women back that we wouldn’t have otherwise."
Cohen’s assessment of CAD is so far anecdotal; he hasn’t used the system long enough to determine how it affects patient management. But in a study published in the September issue of Radiology, researchers from the Women's Diagnostic Breast Health Center in Plano, TX, determined that CAD increases the detection rate of early-stage malignancies without triggering a rash of unnecessary recalls.
Specifically, after screening almost 13,000 women over a one-year period using both conventional mammography reading techniques as well as CAD, the researchers found only a 1.2% jump in the recall rate when CAD was used. At the same time, CAD was responsible for a 19.5% increase in the number of cancers detected, and a 5% increase in the number of early-stage cancers detected (Radiology, September 2001, Vol.220:3, pp. 781-786).
Even with these results, Cohen cautions that CAD isn’t perfect and is no substitute for a good radiologist.
"It would be a mistake to see an abnormality on a mammogram, but ignore it if CAD doesn’t pick it up," Cohen said. "Although it detects a subset of things that are difficult to see, such as tiny calcifications, radiologists seem to be a little better at spotting masses."
In addition, CAD is very nonspecific. It’s programmed to pick up anything that resembles breast cancer, so it detects many anomalies that don’t need additional work-up, Cohen said. On the other hand, CAD is a valuable backup in the sometimes mind-numbing work of reading mammograms: It doesn’t tire, it isn’t interrupted by phone calls, and it reads the edges of films, he added.
To get the best of both worlds, the radiologist first reads the mammograms, and then rechecks suspicious lesions identified via CAD. When this CAD-radiologist dynamic gels, 20% more cancers are detected compared to reading by a radiologist alone, Cohen said.
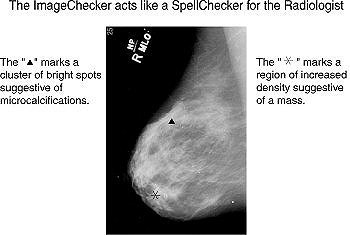 Images courtesy of R2 Technology. |
"The key is to have to have good mammographers who don’t allow the false-positive rate to creep up," Cohen said. "It’s like a fancy jet airplane -- you still need a good pilot."
The ImageChecker CAD system received FDA approval in 1998 for use with screening mammography to assist radiologists in minimizing false-negative readings. In 2001, the FDA expanded approval to diagnostic mammograms. The system, which costs between $145,000 and $229,000 depending on configuration, is installed in about 210 facilities worldwide.
By Dan KrotzAuntMinnie.com contributing writer
October 10, 2001
Related Reading
Computer system helpful in interpreting mammograms, September 20, 2001
Instrumentarium adds CAD deal, September 10, 2001
New CPT code could open door for greater CAD adoption, July 31, 2001
Kodak, R2 extend relationship, July 12, 2001
FDA approves R2 CAD for use with diagnostic mammograms, June 13, 2001
Breast CAD system scores high sensitivity, lower specificity, March 5, 2001
Copyright © 2001 AuntMinnie.com