Dr. Daniel B. Kopans, professor of radiology at Boston-based Harvard Medical School and director of breast imaging at Massachusetts General Hospital, weighs in on the Agency for Healthcare Research and Quality (AHRQ) report, "Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities."
It is my understanding that the U.S. Congress has mandated that government-supported panels, such as AHRQ, cannot include members who have a conflict of interest, and if they have, they cannot be involved in assessing technology and, in this instance, breast imaging technology.
The most recent report by the AHRQ, "Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities," is a clear example of how this is a misguided and dangerous policy. It is clear that not having a conflict of interest also means that you have no expertise in the area. As far as I can tell, there was no radiologist on the AHRQ panel that produced this review, and their conclusions clearly reflect this.
The failure of these authors to understand the basics of breast evaluation can be found in their executive summary. They state: "As a screening test, mammography is used to rule out cancer." This is exactly what mammography cannot do.
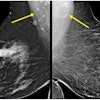
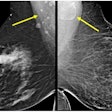
Between 15% and 35% of cancers are not evident by mammography (they are palpable and not visible at the time of screening or become palpable within one year of a negative screening mammogram).
It is dangerously misleading to suggest that mammography is used to "rule out cancer," and it is dangerously misleading for these authors to suggest that diagnostic imaging should be replaced by biopsy for all "suspicious lesions" when this ignores the facts.
Unfortunately, their conclusions will not only confuse women and their referring physicians but will likely, and inappropriately, confuse and mislead insurers who reimburse for breast imaging studies.
The problem lies in the use of the terms "suspicious" and "diagnostic." Many use the term suspicious for any finding on a screening mammogram that needs to be evaluated. Most of these "suspicious" findings prove to be of no consequence and, contrary to this report, these can be safely sorted out using "diagnostic imaging."
For example, approximately 25% of women who are recalled because of a suspicion on a screening mammogram are found to have nothing more than superimposed normal tissue. The authors recommend biopsy of all "suspicious" findings. Do they propose that we biopsy something that doesn't exist?
They have taken the term "diagnostic" literally as in "making a diagnosis." They are correct in suggesting that the imaging tests that they reviewed are rarely able to make a "tissue diagnosis," and, when a lesion is indeterminate and might possibly represent a malignancy, these tests cannot accurately differentiate a benign lesion from a malignant one.
I would agree that PET and scintimammography do not have any established diagnostic value in breast evaluation, but what they have failed to understand is that ultrasound and MRI are very useful in aiding the radiologist in getting to the point where a lesion becomes sufficiently "suspicious" as to warrant a biopsy.
These tests frequently cannot be used to accurately distinguish benign lesions from malignant lesions once the level of concern is sufficiently high, but the authors have skipped the steps before a lesion is sufficiently suspicious, where these tests may be very useful and can safely obviate the need for many biopsies.
The easiest example of this is a woman who is found to have a "suspicious" mass on her screening mammogram. She is asked to return for "diagnostic" evaluation using ultrasound, and the mass is shown to be a simple cyst. Cysts are extremely common. They are not cancer and do not become cancer. Biopsying every cyst, as would be inferred from this report, would be totally unnecessary and, in fact, malpractice.
The AHRQ report needs to be revised. They are correct in suggesting that a biopsy is the only accurate way to determine if a "suspicious" lesion is benign or malignant, but it is the breast imaging radiologist who needs to have other imaging tests available to determine when the lesion is sufficiently "suspicious" to warrant biopsy.
The larger point from this episode is that Congress needs to address its requirement that individuals with a "conflict of interest" cannot serve on these committees. This report is a clear example of how individuals who lack expertise can misunderstand the subject that they have been asked to evaluate.