Computer-aided detection (CAD) markings of mammography images can be discarded by radiologists after they have evaluated the exam and reported their findings. Or can they?
The highly controversial question was raised at the 2005 Computer Assisted Radiology and Surgery (CARS) conference held in Berlin in June.
"No malpractice cases initiated for failure by radiologists to diagnose breast cancer have been won or lost based on mammo CAD documentation," Dr. Matthew Freedman told attendees of a CARS special session on breast CAD. Freedman is a radiologist and an associate professor of oncology at the Lombardi Comprehensive Cancer Center of Georgetown University in Washington, DC, and has experience as an expert witness in malpractice lawsuits.
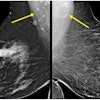
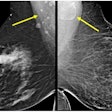
But his statement may not have been 100% correct. There has been one court case, Gray versus Fairview General Hospital in the 8th District Court of Appeals in Cuyahoga County, Ohio, in which a CAD interpretation of a mammography film was introduced into evidence by an expert witness for the defense. The CAD markings, produced at the time of the trial by the expert witness, did not distinguish the cancerous area that the plaintiffs accused the defendant radiologists of overlooking.
The jury returned a finding that the plaintiffs had not proved by a preponderance of the evidence that the defendants were negligent. The degree by which the jury was influenced by the CAD markings is unknown.
The significance of the March 18, 2004, ruling is that a CAD analysis of an x-ray film of a mammography exam is not hearsay, nor is an explanation of the physical observation of CAD markings by an expert witness hearsay.
From the perspective of the radiological community, this case set the precedent of accepting a new technology -- CAD -- into the courtroom and allowing the professional interpretation of CAD to be included as evidence. A detailed, peer-reviewed article about the case and its legal implications is in press for publication in an upcoming 2005 issue of the American Journal of Roentgenology.
The article, "Computer Aided Detection (CAD) Technology in the Courtroom: An Appellate Court's Rulings and Potential Implications," is authored by Dr. R. James Brenner, defense counsel Ronald Wilt, and Dr. Michael Ulissey -- the expert witness who introduced the CAD markings.
No protocol or position paper exists on this topic. The American College of Radiology (ACR) declined to comment or submit a statement to AuntMinnie.com for this article. Brenner, who serves as president of the Society of Breast Imaging (SBI), said that in all likelihood, the SBI may decide to develop a position paper with respect to whether CAD markings should be retained.
Expert recommendations
Freedman recommends that CAD documentation be retained in patients' records.
"In a malpractice case, failure to produce a CAD analysis can give the impression that the radiologist is hiding something," he said. "If you do keep the record, you might be able to show that the area marked was not where the cancer was found. It may have been so indistinguishable that the CAD missed it as well. If you have thrown away the record, you can't prove this."
In cases in which radiologists incorrectly rejected an intermediate mark, they would still be in a better position by saying that they looked at the area carefully, but either did not see the cancer or made a mistake, Freedman said.
"You are better off defending a mistake than you are defending yourself in the absence of data," he said.
Freedman advocates that a radiology practice or hospital establish a policy on CAD documentation, formally document why the policy has been established, and then follow the policy consistently.
"If some CAD markings are saved and others are not, inconsistency will not look good in court," he said.
CAD markings become a matter of the medical record once they are used to assist in the interpretation of a mammogram by a radiologist, according to Gerald R. Kolb, J.D., president of breast center economics consulting firm Breast Health Management of Bend, OR.
If the CAD marking is printed on paper and utilized for interpretation, the paper should be saved to the file as part of the medical record, Kolb said. Saving the paper printout may also be important to some users as a billing record to prove that an invoiced CAD was actually performed. In the case of digital mammography, if the "For Processing" image is not saved to the data storage system, Kolb recommends that the digital CAD overlay be stored.
"Digital data is 100% reproducible, but a practice may only save the processed image," Kolb said. "With the exception of GE Healthcare's digital mammography systems, CAD algorithms use raw images, not processed images. If the preprocessed image is saved, it is important that the same CAD algorithm be available at a future date. Different software versions of CAD may produce different results as they are steadily improved."
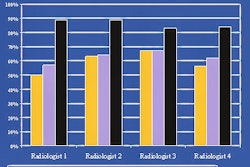
Kolb also noted that since CAD systems are now about 97% effective in identifying cancerous areas, radiologists who do not use CAD may find themselves being asked in a malpractice lawsuit why CAD was not utilized.
"Does a radiologist say to the plaintiff's attorney that he didn't feel it was worth the money to purchase?" he said. "Does he say that he can make as accurate an interpretation without using it, citing the results of published clinical trials that CAD has a variable impact on the interpretation process by radiologists on some radiologists' findings as it does on others, and that he is one of those radiologists for whom CAD is not that helpful? Either way, the jury won't buy it."
Kolb said that the medical profession is not doing an effective job in making it known to patients that cancers can be extremely difficult to identify and do get missed.
"The risk of being sued for a missed cancer is high," he said. "But getting sued does not mean that a radiologist will be found guilty of malpractice. A radiologist who can prove he has done as much as possible to prepare to read mammograms accurately and uses the best available equipment will have a stronger case. Today, among other things, this means using CAD."
Juries do not accept the concept of an "honest mistake," said Dr. Leonard Berlin, chairman of the department of radiology at Rush North Shore Medical Center in Skokie, IL.
"If CAD marks an area where cancer develops, a jury will assume the radiologist erred in judgment," he said.
Berlin advocates that radiologists follow professional standards and protocols. But as of now, there's been no mandate from either professional societies or state laws on how to handle CAD markings.
"CAD is a tool to assist a radiologist in interpreting a mammogram," he said. "It is the decision of a radiologist to determine if an area marked by CAD should be further investigated or the patient should be recalled. A radiologist who utilizes CAD needs to document that the CAD was used in his or her radiology report. Once this report is signed, the radiologist is under no obligation to retain the CAD -- until or unless the law or professional standards change."
This advice is practiced by the majority of the customers of one CAD vendor, R2 Technology. R2's principal engineer Julian Marshall believes that over 8 million CAD interpretations have been discarded.
The use of CAD is part of the diagnostic component of a mammography exam, said Thomas Greeson, a healthcare attorney affiliated with law firm Reed Smith in Falls Church, VA.
"The outcome of an exam is the radiology report," Greeson said. "If CAD is used, the findings should be thoroughly documented in the report. But there is no legal or professional requirement to save the CAD."
Both Greeson and Berlin noted that a growing body of professional literature has been published showing that CAD processing of film is not 100% reproducible, even when using the same software algorithm version and the same film digitizer.
Greeson described a hypothetical scenario in which a film may be processed with CAD several times, yet mark a specific microcalcification only once. Years later, how can this be accurately reproduced?
"It can't. The software is different. The digitizer is older and different, or replaced entirely," Greeson said. "The radiologist may have retained the one out of several CAD printouts that caught the subtlety of a microcalcification in an area of the breast where cancer would develop. How could the radiologist even try to prove that the CAD printout he diligently retained may have been a CAD exception rather than the rule?"
Brenner, who's also director of breast imaging at the University of California, San Francisco, School of Medicine, noted that many radiologists equate CAD markings to that of a "smoking gun." It is not the CAD mark that determines the standard of care, although a plaintiff's attorney in a malpractice lawsuit would like to claim so.
"The standard of care is based on the judgment of a reasonable and prudent radiologist in not recalling a particular lesion for additional imaging or biopsy, not the fact that a CAD mark was there," Brenner said. "Although the accuracy of CAD algorithms improves with each new software version, they still generate a large number of false positives. Most CAD programs do best with clustered calcifications, well but not best with masses, and not very well with architectural distortions. But CAD also misses cancers that, as studies have shown repeatedly, the radiologist can identify."
Radiologists are responsible for evaluating the entire image, Brenner said.
"If the mark attracted their attention and they deliberated on the mark and decided not to recall, they are responsible for that decision," he said. "If a diagnosis requires a different type of procedure -- an ultrasound or a breast MRI -- it should be ordered."
Brenner pointed out that CAD marks are an aid to serve as a "check" or "second look" for a radiologist. Because most of these marks are not associated with recallable lesions, there is no standard of care issue that the radiologist has to recall the patient.
Spoilation
Arguing in favor of keeping CAD markings, Brenner believes that if a radiologist destroys a CAD image, the plaintiff will argue in a malpractice lawsuit that the radiologist threw the evidence away. Spoilation usually has a negative impact on a jury.
And if radiologists believe the CAD was a factor in the basis upon which they made their best interpretation, then the original image, like a screen film, should be kept to support their defense and professional standard of care, Brenner said.
Dr. Richard Anderson, chairman and CEO of the Doctors Company, the leading physician-owned medical malpractice insurance provider, said that in 2001, he predicted that CAD, despite being a potentially significant clinical advantage, was going to become a "medicolegal can of worms."
"In the legal context, there is no safe harbor except perfection," he said. "That is what juries expect. If a radiologist uses CAD because it is clinically proven that this technology can detect more cancers, and the radiologist doesn't use it perfectly, he's damned. If a radiologist doesn't use it, he or she may be damned for not using a technology that could have detected the missed cancer. Similarly, retaining a CAD overlay can work both for and against a radiologist."
"We advise our policyholders to use their best judgment," he said. "We warn that if a radiologist has a false-negative mammogram for breast cancer, he or she is likely to face litigation. Retaining a CAD overlay can support the radiologist or can harm him."
It would be helpful for this profession to set standards, Anderson said.
"CAD is proven to save lives," he said. "It is here to stay."
By Cynthia Keen
AuntMinnie.com contributing writer
September 1, 2005
Related Reading
Part II: Computer-aided detection identifying new targets, July 15, 2005
Part I: Computer-aided detection identifying new targets, July 14, 2005
VC CAD shows progress toward clinical use, June 3, 2005
CAD struggles through tagged, subtracted VC data, May 18, 2005
Support vector machines boost accuracy of VC CAD, May 3, 2005
Copyright © 2005 AuntMinnie.com