Mammography is tough -- just ask any radiologist, technologist, administrator, or patient. This anxiety-provoking exam provides every participant the distinct sense of playing biological roulette. For a healthy woman, a mammogram is an annual reminder of a potentially deadly disease, with a 2% to 10% chance of obtaining a category 0, 4, or 5 result that leads to either nerve-racking further workup or the diagnosis of cancer.
For the radiologist, mammography poses a constant malpractice threat. For the technologist, it presents an inherent conflict -- more compression means a better mammogram but a less happy patient. For the administrator running an imaging center or hospital, mammography is almost always a money-losing proposition that tests one's commitment to comprehensive medical imaging. But despite all this, mammography is wonderful because mammography saves lives and decreases morbidity. God bless mammography.
Basic opportunities of soft-copy reading and digital mammography
Digital mammography provides some hopeful solutions. The theory on which digital mammography is based is that a better digital image will result in more sensitive and accurate breast cancer diagnosis. After more than a decade of research, however, one cannot state that this theory has been proved.
In my opinion, the greatest potential benefit of digital mammography with soft-copy reading will not come from better image quality per se. It will come from a more transportable image, leading to greater access to mammography experts, as well as from image presentation methods that inherently improve the human detection of lesions and efficiency of reading.
Is access to mammography experts an important issue? Most definitely, the answer is yes.
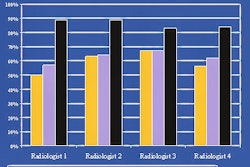
Radiologists vary tremendously in their rate of detecting biopsy-proven breast cancers per 1,000 mammograms read. The literature suggests a variation of between two and six biopsy-proven cancers per 1,000 depending on the reading radiologist.
I have gathered unpublished data from multiple radiology groups (the data that the Mammography Quality Standards Act [MQSA] requires you to maintain, but does not require you to act on), and my observation is that the number of biopsy-proven breast cancers per 1,000 mammograms read among different readers in the same radiology practice varies from one to 15.
This means that in the same practice a woman's chance of having a breast cancer detected can vary by as much as 1,500% depending on who reads her mammogram! It is a staggering figure. Consider, in contrast, the relative value of mammography computer-aided detection (CAD), which increases breast cancer detection by 7% to 9%, is a reimbursable item, and is routinely used to market the quality of a mammography practice.
Film-based mammography inhibits expert reading simply because film is inconvenient and expensive to transport to experts within a group or community. Similarly, the requirement of manual transport of prior mammograms for comparison reduces the likelihood and increases the cost of comparing results to prior mammograms.
Finally, expert readers presumably read more accurately, at least in part, because they have developed search methods and perceptual patterns that work better. With film-based mammography, it is nearly impossible to even study this process. In contrast, soft-copy reading provides the unique opportunity to structure image and information display and reporting in ways that inherently lead to more sensitive and accurate detection.
Soft-copy reading and radiologist efficiency
Whereas soft-copy reading increases efficiency with imaging modalities other than mammography, studies to date suggest that soft-copy reading reduces radiologist efficiency for digital mammography. Why?
Mammography provides unique challenges for soft-copy readers and vendors that supply mammography PACS. The images are large matrix, so that a single digital mammography image often is not completely displayed on even a 5-megapixel (MP) monitor, the current U.S. Food and Drug Administration standard.
Digital mammography images today vary from 2,000 pixels to approximately 4,000 pixels per linear dimension, and new computed mammography products in development promise single mammographic images of up to 8,000-9,000 pixels per dimension. As a result, display of each pixel of even a single mammographic image on a 5-MP monitor (2,000 x 2,500 pixels) requires manual image manipulation.
There are two basic options for displaying all pixels of a mammographic image, henceforth referred to as full-pixel display. With one option, the mammographic image must be clipped, and the reader appropriately pans to each portion of the image for full-pixel display.
Alternatively, the image may be displayed without clipping, such that only a fraction of the pixels are simultaneously shown, in which case selected areas of the nonclipped image may be manually displayed at full resolution by panning a magnification tool around each image area. Whichever strategy is selected, the risk is high that the reader will fail to display each pixel of each image, which paradoxically is most important when evaluating mammograms because a single pixel may represent a suspicious calcification.
Further compounding the problem is the need to typically compare four to six projections of the current bilateral mammogram to comparable views of one to four, or more, old exams. Stated simply, even with a multiple-monitor viewing station, there simply is not enough display space to conveniently exhibit 12 or more mammographic images at full resolution without a significant paradigm shift compared with the film viewbox display.
Tools and methods for soft-copy viewing of mammograms
Several software tools have been introduced to facilitate efficient viewing of all the pixels of a digital mammogram. Before describing these tools, let's define a few terms:
Shrinking: This condition arises when an image contains more pixels than are simultaneously available in the allocated space on a monitor. Image shrinking results in a display of the entire dimension of the image, but a fraction of the pixels are not displayed. For example, when a 4K x 4K-pixel image is displayed on a 2K x 2K monitor with image shrinking, the image is not clipped but only every other pixel is displayed at full resolution (meaning three of four total pixels are not displayed).
Clipping: This condition arises when an image contains more pixels than are simultaneously available in the allocated space on a monitor. In this condition, some of the image along the upper, lower, left, or right image border is omitted from display.
Software tools to enhance full-resolution display
Shrink on or off: This tool is facilitated by a hot key or other shortcut. It is typically used when the image matrix exceeds the number of pixels available in the display area. This tool enables the user to quickly toggle between full-resolution display (shrink off, typically resulting in image clipping) versus display of the entire image (shrink on, typically resulting in a display of a fraction of the pixels in an unclipped image).
Magnification box: This presents a box of variable size within a shrunken image. The size of the magnification box may be modified. The area of the image within the box is displayed with shrinking off, so that all pixels are displayed, no matter what the matrix size is of the image. The box may be panned around an image to display all the pixels in the image.
Mirrored and nonmirrored panning: Panning offers simultaneous controls of the display of neighboring clipped, full-pixel display images, such that when panning one image to display the otherwise clipped regions, the neighboring image moves synchronously, either in the same direction or in a mirrored direction.
Mirrored and nonmirrored magnification box: This simultaneously displays a magnification box within two or more neighboring images such that panning of the box in one image results in synchronous panning of the box in one or more neighboring images, either in the same or a mirrored direction.
Scrolling: This tool sequentially shows multiple images in the same display area. Scrolling has become a very popular and common method for soft-copy reading of MR and CT slices, and is also gaining popularity with other modalities. The theoretical benefit is improved perception, particularly the capability to note changes between sequential images displayed in the same area, in contrast to side-by-side comparison.
Scrolling through time: This type of scrolling enables viewing of comparable images from multiple different exams performed at different times on the same patient. For example, instead of scrolling through multiple slices of a single CT exam, it offers image scrolling through multiple craniocaudal views of a left breast mammogram on different dates, going back through time. By displaying the same view in the same area, perception of subtle changes over time may be enhanced, and monitor space may be used much more efficiently.
Series-linked scrolling: This tool offers scrolling, including scrolling through time, of two image series simultaneously. The linking process can be manual or automatic -- on the basis of cursor position, series naming, or DICOM criteria. In mammography, this may result in scrolling through time of left and right breast mammographic views in neighboring display areas.
Image shuffling: Shuffling involves instant creation of an image series that is comprised of two or more distinct image series. An easy way to imagine this is to consider a deck of cards. Imagine there are four image series, representing each suit in the deck. One could scroll through the hearts, diamonds, clubs, and spades separately or synchronously via series-linked scrolling. With shuffling in this example, however, the four image series are instantly shuffled so that a new virtual series is formed containing all 52 cards.
Scrolling results in the display first of the aces, then twos, then threes, and so on, with the order of the suits and the precise placement of the shuffle controlled by the user interface. Image shuffling in mammography enables the instant creation, for example, of a series containing all the left views of multiple sequential exams on the same patient, so that scrolling displays the new then older left craniocaudal views in the same display space, followed by the new then older left oblique views in the same display space.
Multiple simultaneous shuffling: This involves shuffling to create multiple new shuffled series. In mammography, this can result in side-by-side display of appropriate left and right views of the same exam, with each side-by-side display area holding a shuffled series of appropriate left and right images from multiple chronological exams. This results in a dramatically more efficient use of monitor space to display new and old exams in a stack mode of reading.
Jump to 1:1 display: This tool enables the designation of one or more series that are arranged on a 2 x 1 or higher multiformatted matrix on a monitor, such that with a single mouse click, the display is instantly changed to a 1:1 format per monitor, with display of the designated series. In mammography, this jump to 1:1 enables the user to display many image series on a monitor, then quickly jump to 1:1 display (which may be combined with shuffling, scrolling, or simultaneous shuffling), so that full-pixel display is more rapidly achieved.
Cursor position-based action initiation (CPAI): This methodology may apply to any of the tools noted above or other image management tools. CPAI means that the software recognizes the cursor position relative to multiformatted image display, and initiates a different action on the basis of different cursor positions. For example, placing the cursor near the border between two image series may initiate scrolling of both series. Placing the cursor near the border may similarly result in multiple simultaneous shuffling, mirrored panning, and so on. CPAI improves speed of review and radically reduces mouse clicks.
Image organization controls: These controls enable image organization into series in ways that enhance display efficiency, such as consistent ordering of images within a series based on the mammographic view (for example, display of craniocaudal view first, then oblique) and consistent ordering of the display of image series (such as the left series displayed with priority over the right).
Pixel tracking: This capability enables the user to interactively determine if image areas have been displayed with full-pixel display. With a single click or hot key, the user can determine if any image area has not been fully displayed and can then display that area. Pixel-tracking rules can be established based on criteria other than full-pixel display (such as 75% pixel display, or display with a certain window/level). This helps ensure that all images are fully evaluated.
Compare mode: This mode automatically organizes the display format of new and old exams such that appropriate image series are displayed side by side or above-below.
Preloading of exams: This automatically fetches from an image server appropriate exams based on user-designated rules linking exam types, so that exams can be rapidly displayed without waiting for transport across a local or wide area network.
Soft-copy reading regulatory issues
After extensive communication with the FDA over the previous three years and review of published policies, the following represents my understanding of current U.S. regulatory requirements in specific areas where questions often arise.
Monitors used for soft-copy reading: Only 5-MP or higher matrix monitors that have been approved for digital mammography can be utilized. Maintenance must follow the manufacturer's instructions.
Data compression: Lossless data compression can be used for primary reading and primary archive, but no lossy data compression is permitted for these purposes. Lossy data compression can be used to transmit images for viewing by referring doctors. Any compressed image should be labeled appropriately.
Digitizers: Prior mammograms may be digitized for comparison, and lossy data compression may even be applied for the comparison exam. Basically, the FDA does not provide tight regulation as to how the prior exam is viewed. Digitizing prior film-based exams for comparison purposes may improve reading efficiency, and may reduce the inherent problem of veiling glare when trying to compare one exam on a monitor to another exam on a viewbox.
Digitizing for archive: A film mammogram cannot be digitized as the only form of archive. The original mammographic image must be stored for 10 years. As noted above, a film-screen mammogram can be digitized and even compressed in addition to storing the original. It seems likely that this digitized version would suffice for comparison in the majority of exams, except perhaps for those exams where a subtle finding is newly detected, and one wishes to scrutinize the original prior exam before concluding with certainty that the finding is truly new. Assuming a digital copy of a film mammogram suffices for comparison purposes in most exams, this may reduce labor costs associated with archive and retrieval of film mammograms.
Printing digital mammograms: Only printers specifically cleared by the FDA for mammography may be used to print digital mammography images.
Mammography reporting and coding: MQSA requirements are fully detailed at the FDA Web site, including mammography reporting and coding requirements. Soft-copy reading that integrates computerized reporting and tracking can potentially reduce costs and greatly improve the efficiency of readers.
Other breast imaging modalities
Breast cancer detection and staging increasingly involves other imaging modalities, including ultrasound, MRI, and PET. Soft-copy reading can greatly enhance the capacity for comprehensive breast imaging care by making all studies available on the same system.
Dynamic contrast-enhanced breast MRI: Of the many tools discussed above, image shuffling may have the most profound effect on viewing breast MR images. Typically, within a breast MRI exam, at least four image series are obtained during dynamic contrast enhancement. Detecting breast cancer requires the reader to perceive inflow and outflow of contrast into each anatomic position. With appropriate image shuffling, scrolling through time, displaying each anatomical slice in sequence during contrast perfusion, can potentially improve the perception of contrast-enhancing lesions.
In addition, several proprietary software analysis programs are now available to facilitate parametric analysis of dynamic contrast-enhanced breast MR images.
Breast ultrasound: One feature of the DICOM standard is a technology called DICOM multiframe. This technology enables storage and display of real-time cine clips -- more specifically, a series of images obtained rapidly during an ultrasound exam. Support of DICOM multiframe technology by the PACS vendor and ultrasound manufacturer is essential.
Until now, computerized image display of digital mammograms has tended to mimic preceding methods of viewing film mammograms on a viewbox. Many new technologies now promise to shift the paradigm, resulting in faster, more accurate image review, with built-in reporting, tracking, and even teaching file capabilities.
By Dr. Murray Reicher
AuntMinnie.com contributing writer
July 21, 2005
Dr. Reicher is a practicing neuroradiologist and chairman of San Diego-based RIS and PACS developer DR Systems, as well as chairman of imaging center operator Radiology Service Partners, also of San Diego.
Related Reading
PET mammography unit shows promise for DCIS, June 22, 2005
RT bears burden of QA failure at PA mammo clinic, June 9, 2005
PA mammo clinic fails QA, must pay for re-screens, June 9, 2005
IOM advocates more monitoring of ailing mammo services, May 27, 2005
Breast imaging trends show longer waits for screening mammo, more biopsies, May 6, 2005
Copyright © 2005 Murray Reicher, M.D.