AuntMinnie.com spoke with two of the Radiology study authors, as well as outside legal counsel, on the further ramifications of this research.
The following offered their thoughts on the study findings:
Lead author Dr. Joann Elmore, an associate professor of medicine and an adjunct associate professor in epidemiology at the University of Washington in Seattle. Elmore is also the section head for general internal medicine at Harborview Medical Center and an associate director of the Robert Wood Johnson Clinical Scholars Program, also in Seattle.
Co-author Dr. Carl D'Orsi, a professor of radiology, hematology, and oncology at Emory University in Atlanta. He is also the director of the Breast Imaging Center at Emory.
Maggie Finkelstein, an associate attorney in the health litigation group at Stevens & Lee in Lancaster, PA.
Were you surprised by the results of the study?
Elmore: We expected to find a high level of concern about medical malpractice, but the extent was impressive and more than anticipated. Failure to detect breast cancer has been one of the most common allegations in medical malpractice cases over the years. This is an important area where litigation may be adversely impacting clinical care and needs to be addressed. Women in the U.S. may be getting more breast biopsies than in other countries because of a fear of a future suit if a cancer is missed.
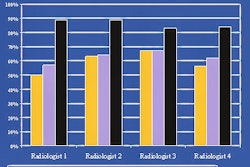
D'Orsi: I think we were expecting to see some association between personal malpractice experience and recall rates, biopsies. However I think the situation regarding malpractice is much worse given the fact that more than one-third considered leaving mammography because of malpractice. This tells us that almost all readers are thinking about malpractice and all are probably reading defensively, to some extent, which is why we did not get a subset difference.
Elmore: Carl mentioned the fact that we did not find a direct association between the survey results and the actual performance in clinical practice (since we had linked community data to [the radiologists'] survey responses). This might be due to the fact that the majority of radiologists had high recall rates, and our survey question had only a five-point scale, with all of the radiologists responding in the 4 and 5 category, stating that they were very concerned (about malpractice), with no one answering that they were not concerned -- we asked the question both ways to be thorough.
The study states that "radiologists believed that their peers' recommendations are more influenced by malpractice concerns than their own recommendations" (Radiology, July 2005, Vol. 236:4, p. 40).
Despite all the negative media attention mammography receives, is it possible that radiologists are somewhat in denial as to how litigation can impact their practice, i.e., "That only happens to other people, not me"?
D'Orsi: This is a very complex issue that goes into interpreters' personalities, etc. When we look at someone else's request for recall and/or biopsy at times we may say, "Boy, I never would have recalled that," or "Who would biopsy that?" The thinking, however, does change when your name is on the bottom of the report. Quite the contrary, I think when you're responsible for an interpretation the thinking may be "That can easily happen to me."
Finkelstein: Certainly this study shows that while the radiologist may perceive that his or her peers may be practicing "defensive medicine," they (the radiologists studied) are also.
From a purely legal standpoint, what are the pros and cons of the results of this study?
Finkelstein: This article could be very helpful in preventing lawsuits in the first place. Sharing this type of data is important and has a value in expressing to radiologists, their staff, hospitals, and administration the effects that litigation has on the radiologist and the radiologist's practice. For example, it certainly shows that a majority of radiologists who have been involved in medical malpractice litigation find it to be a very stressful experience. As we know, the data shows that this has an effect on patient care, the office environment, and certainly the practice's bottom line.
We know that lawsuits can be prevented with the pursuit of best practices in both clinical risk and risk management. Studies such as this can help solidify the reasons for pursuit of risk management practices like communication and service excellence, and the value of the same.
Furthermore, when ordering mammograms or breast biopsies, it is important to remember to do so when clinically indicated. If we are practicing defensive medicine, we can actually go in reverse, exposing radiologists to liability risks such as complications from unwarranted procedures and false positives.
Although there was no direct association between reported malpractice concerns and recall rates, did the physicians offer any comments as to why they think recall rates have continued to rise?
Elmore: See our paper, "International Variation in Screening Mammography Interpretations in Community-Based Programs." We outline reasons for the high recall rate in the U.S. compared to other countries (Journal of the National Cancer Institute, September 17, 2003, Vol. 95:18, pp. 1384-1393).
Do you think the use of new technologies, such as computer-aided detection (CAD) or full-field digital mammography (FFDM), could potentially alleviate the perception of litigation risk?
D'Orsi: If we used CAD to alleviate the concern of malpractice, then we would have to act on every mark these systems make. So if something does occur, you can say, "Well, I checked out every mark the system made." Of course this would dramatically increase recall.
On the other hand, as lawyers get more versed in CAD, marks (may be) used in court against the defendant. Or the records of your own CAD may be subpoenaed, and correctly ignored marks can then come into question down the road. The job of the plaintiff's attorney is to contort the truth to his advantage, which is easy to do with CAD. The (American College of Radiology) predicts that we will see more malpractice cases involving CAD in the near future.
Digital mammography should not alleviate one's fears since there is, at this point, sensitivity equivalency for FFDM and film-screen mammography.
Do you plan to do any follow-up with these respondents, particularly those who said they were seriously considering withdrawing from reading mammograms?
Elmore: Yes. We hope to survey community-based radiologists this fall to find out what their thoughts are on the high level of auditing and reporting that the government requires (through) the Mammography Quality Standards Act (MQSA).
By Shalmali Pal
AuntMinnie.com staff writer
June 28, 2005
Related Reading
Breast rads believe malpractice fears prompt more recalls, June 28, 2005
Medical malpractice premiums rise more than awards, June 1, 2005
JAMA study: 'Defensive medicine' fuels unneeded imaging exams, May 31, 2005
IOM advocates more monitoring of ailing mammo services, May 27, 2005
Copyright © 2005 AuntMinnie.com