Calcific tendinitis of the shoulder is caused by carbonate apatite crystal deposits in the rotator cuff tendons. In about half the patients who suffer from this condition, the deposits can become symptomatic, causing pain. But the good news is that this is a self-limited disease process that will resolve on its own. During the self-healing process, the pain can be intense, so orthopedic experts are on the hunt for pain management methods.
Three groups of researchers, one based in Germany, one in Bangladesh, and the other in Spain, looked at the role of ultrasound in calcific tendinitis of the shoulder, both as a preoperative test and a treatment modality.
Presurgical US
The success of arthroscopic surgery for calcific tendinitis depends largely on localization of the calcium deposits. Unfortunately, these deposits are not easy to find intraoperatively, according to investigators from the Klinik für Unfall-und Wiederherstellungschirurgie in Berlin.
"Failure to locate the calcium deposit can make the surgical process extremely frustrating and may result in a very long operative time," wrote Dr. Ralph Kayser and colleagues. "Our study demonstrates that preoperative ultrasound-guided marking of calcium deposits significantly enhances the clinical results or arthroscopic removal of calcium deposits.... This procedure is now routinely used at our hospital for removal of calcium deposits" (Arthroscopy: The Journal of Arthroscopic and Related Surgery, January 2007, Vol. 23:1, pp. 43-50).
A total of 24 patients with calcific tendinitis were randomly assigned to two treatment groups: those who underwent preoperative ultrasound-guided marking (pre-USM) and those who did not. Static and dynamic ultrasound studies of both shoulder joints were done by the operating surgeon.
The transducer position was marked on the skin in two planes with the junction of the two transducer markings representing the point of maximal sonographic echogenicity of the calcium deposit. This junction was used as the intraoperative insertion site for the needle.
Postoperative x-rays were obtained and follow-up sonographic exams were done six and 12 weeks postoperatively. Of the 24 patients, 92% were available for follow-up two years later.
According to the results, nine of 12 patients in the pre-USM group showed excellent or good clinical results, and three rated the outcome as satisfactory. Residual calcium deposits were seen on ultrasound in two cases. Revision surgery was unnecessary.
In the second group, clinical results were deemed satisfactory in three of 12 cases, sufficient in one case, and poor in two cases. Four patients had residual deposits upon x-ray and ultrasound exams, two of whom required reoperation.
In the pre-USM group, the average surgical time was 90 minutes versus 104 minutes for the second group. In the pre-USM arm, postoperative ultrasound exams showed textural changes in the tendon with no signs of calcium deposits in eight cases. In group 2, six patients had no sonographic signs of calcium deposits after surgery. In four cases, residual calcium deposits were clearly visible.
"Complete removal of calcium deposits correlates with good or excellent clinical results," Kayser's group concluded. "Preoperative ultrasound-guided marking of calcific deposits is a procedure that enhances ... the clinical results of arthroscopic surgery."
They emphasized that any pre-USM protocol should be carried out with the patient's arm and shoulder in the same position as during surgery. Also, in terms of the marking procedure, they recommended tracing the full outline of the transducer in two planes over the calcium deposit's site of maximum echogenicity.
US-guided lavage; UST
Shockwave therapy is one effective treatment option for calcific tendinitis, but it's expensive and surgery is generally considered a last resort, according to Dr. Jose Luis del Cura and colleagues. Instead, this group of radiologists, surgeons, and rheumatologists recommended sonographically guided percutaneous needle lavage, which they tested out in a recent study published in the American Journal of Roentgenology.
For their study, the authors -- practicing at the Hospital de Basurto and Basque Country University, both in Bilbao, Spain -- included results from 67 shoulders in 65 patients, all of whom had been diagnosed with calcific tendinitis. Patients underwent pretreatment x-ray and sonographic exams. Discomfort was measured with the Shoulder Pain and Disability Index.
For imaging and ultrasound guidance, a linear 5- to 12-MHz transducer was used on one of two units (ATL HDI 3500 or ATL HDI 5000, Philips Medical Systems, Andover, MA). Lavage of the calcifications was done following the plane of the ultrasound beam with the needle connected to a syringe filled with 1% lidocaine hydrochloride. The volume of the calcium extracted was measured. Patients were followed up at five weeks, 10 weeks, and one year. The mean time from symptom onset to treatment was 30 months.
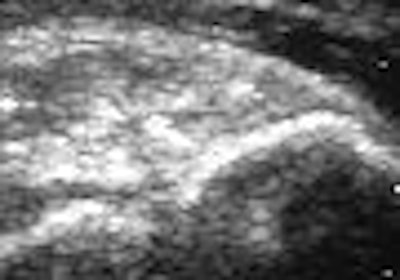
 |
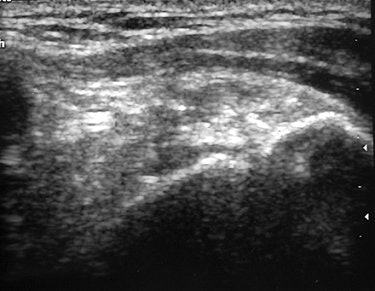
| A 39-year-old woman with calcific tendinitis for six months. Before treatment, longitudinal sonogram of supraspinatus tendon shows focus of calcification and acoustic shadow. |
According to the results, the suprasinatus tendon was involved in 57 of the 67 shoulders. In 83.6% of the cases, radiographs showed dense, homogenous, and well-defined calcifications. All calcifications were visible on sonography with 58.2% demonstrating a strong acoustic shadow. In terms of calcium extractions, the mean volume per patient was 0.4 mL with no calcium extracted in 25% of the subjects.
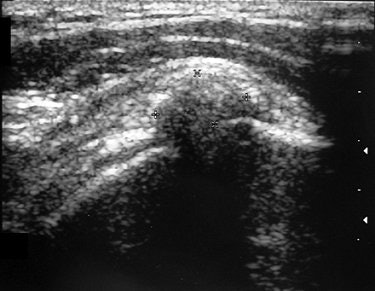
At one-year follow-up, post-treatment radiography indicated that 78.1% of the shoulders showed no sign of calcifications. Before treatment, 58.2% of the cases had strong acoustic shadows on sonography, but after one year only 1.6% showed a strong acoustic shadow. A little over half (50.7%) of the shoulders were completely free of symptoms, the authors reported. These patients also reported lower scores on the Shoulder Pain and Disability Index.
 |
| Same patient as above. Note changes in sonogram of calcification after percutaneous treatment. Ten weeks after treatment, volume of calcification has been considerably reduced and no acoustic shadow is seen. Del Cura JL, Torre I, Zabala R, Legórburu A, "Sonographically Guided Percutaneous Needle Lavage in Calcific Tendinitis of the Shoulder: Short- and Long-Term Results" (AJR 2007; 189:W128-W134). |
Complications during initial treatment included loss of consciousness and seizures. To combat the latter, the authors added an anxiolytic to the treatment regimen. Additional treatment was required in 16 of the 67 shoulders.
The authors noted that "nearly half of our patients experience a recurrence approximately 15 weeks after treatment; the recurrence is usually temporary and lasts an average of six weeks" (AJR, September 2007, Vol. 189:3, pp. W128-W134).
Nevertheless, "to our knowledge, our results have been better than those reported in any previously published reports of percutaneous needle aspiration and lavage," they stated, crediting their technique for bringing about these improved results. The authors explained that they chose 20-gauge needles to avoid needle obstruction. In addition, they did not do double injections and only used one aspiration and lavage procedure per calcification.
In an earlier prospective study, Dr. M. Habibur Rahman and colleagues at the Dhaka Medical College in Dhaka, Bangladesh, also had luck with ultrasound therapy (UST) in calcific supraspinatus tendinitis. "This condition is sometimes mistaken for impingement syndrome or adhesive capsulitis," wrote Rahman and co-authors including radiologist Dr. Md. Sarwar Ramiz, leading to the wrong kind of treatment, they added (Mymensingh Medical Journal, January 2007, Vol. 16:1, pp. 33-35).
But once the diagnosis was made on imaging in their patient population of 26 people, straight UST (without percuntaneous needle aspiration) offered an inexpensive and relatively simple treatment option. For this study, UST was administered for 10 minutes per session to the area over calcification at 1 MHz/cm. Overall, UST doses were given every other day until a maximum of 12 treatment sessions was attained. Intensity of pain was measured six and 12 days after treatment. The authors reported that all patients were free from pain and restricted shoulder movement post-UST. X-rays in 24 cases showed no calcium deposits.
In an interesting footnote, the majority of the patients in this group (46%) were diabetic. The authors pointed out that insulin-depending diabetics tend to suffer from calcific supraspinatus tendinitis more frequently than the general population, most likely because of an inadequate vascular supply to the affected area.
By Shalmali Pal
AuntMinnie.com staff writer
September 4, 2007
Related Reading
US-guided interventional procedures boost sports medicine performance, May 3, 2007
US shows full spectrum of shoulder injuries, September 29, 2006
Copyright © 2007 AuntMinnie.com