SAN FRANCISCO - Some facilities, and even a few researchers, have begun to favor the growing diagnostic capabilities of multidetector-row CT over MRI for assessing bone lesions. And they are daring to ask if CT might have advanced enough to take on MRI's robust characterization of many musculoskeletal pathologies.
The answer, according to Dr. Garry Gold, assistant professor of radiology at Stanford University School of Medicine, is that CT is sometimes better, MRI excels in other areas, and occasionally the two modalities are complementary.
"If you're interested in cortical bone, CT is obviously the way to go," Gold said in a presentation Thursday at the International Symposium on Multidetector-Row CT. Soft tissue or marrow you want to use MRI, and occult fracture both, although I think MRI is still somewhat more sensitive."
Even the presence of hardware in the patient doesn't rule out the use of MRI, he explained in an e-mail to AuntMinnie.com.
"I choose MRI in hardware settings when there's not a lot of hardware and I'm concerned about the nearby tissues," he wrote. "For example, if the question is osteomyelitis, MRI with STIR sequences can still show marrow edema near the hardware. For hardware failure and for fracture healing, I choose CT."
In his presentation, Gold used several case studies from Stanford to illustrate his assessments. First up, a basketball player with foot pain.
CT (0.5-mm reconstructions) revealed only subtle sclerosis of the navicular bone. But MRI showed a region of low signal on T2- and T2-weighted images, surrounded by marrow edema within the navicular bone. "In this case MRI is still somewhat more sensitive (for occult fracture) probably due to the presence of marrow edema," Gold said.
 |
| In a basketball player presenting with foot pain, MRI (below) was better able to show an occult fracture of the navicular bone. All images courtesy of Dr. Garry Gold. |
 |
In another patient, a fracture through the inferior glenoid was fairly obvious on both MRI and MDCT, although the surgeons specifically asked for 3D CT images to help plan the surgical approach to repairing the large Bankart lesion, Gold said.
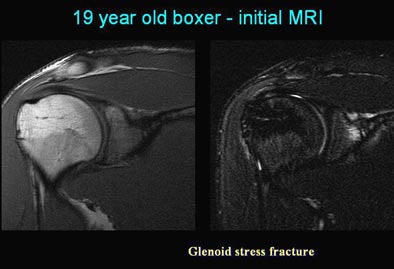
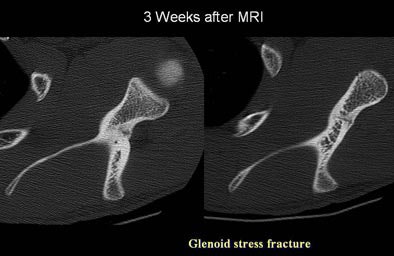
Then there was the 19-year-old boxer who had spent too much time at the punching bag.
"MRI T1 and T2 showed marrow edema in the neck of the glenoid along with a low signal fracture line, and here on these oblique sagittal images we see all this marrow edema within the neck of the glenoid," he said. "And I think at this point the difference between CT (3-mm reconstructions) and MRI is this sensitivity to marrow edema that you see on MRI."
 |
 |
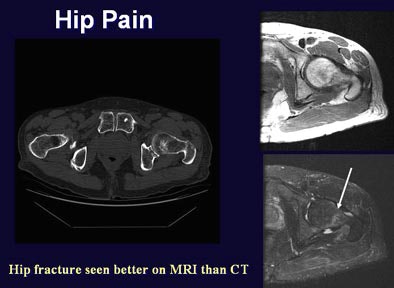
Another patient, presenting with hip pain after trauma, underwent CT of the pelvis. But the fracture was extremely subtle on CT, Gold said. A subsequent MRI exam appeared to show a cortical break in the femoral neck on the left side, as a fracture line with marrow edema in that region, Gold said. The diagnosis was occult femoral neck fracture that was very difficult to see on CT.
 |
"So I think for fractures, if you have a choice, I would go with MRI," he said. "CT is still very good."
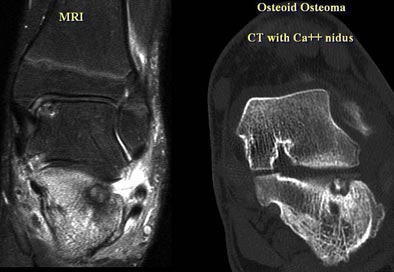
In an 18-year old presenting with foot pain, MRI showed diffuse marrow edema throughout the calcaneous on axial T1 and T2 MRI images, Gold said. But CT (0.5-mm reconstructions) was needed to adequately characterize the lesion, clearly showing a calcified nidus, Gold said. The diagnosis was osteoid osteoma of the subtalar joint.
 |
Finally, MRI beat CT in the case of another student, who came back from a ski trip with a knee injury. MDCT (1-mm reconstructions) showed only a vague sclerosis in the lateral femoral condyle, Gold said. On the other hand, proton-density fat-suppressed MRI image showed a marrow lesion in great detail. The lesion was lymphoma, biopsied under MRI to achieve better localization.
 |
"If bone and not marrow is the key issue, multidetector CT is usually the best choice -- and also for speed, we use it in trauma," he said. "MR is a little bit more sensitive for occult fractures, but MDCT is still quite good. If bone is not the key issue, then MRI is usually the best choice, because you get a little better look at the soft tissues around the joint. And if MRI is contraindicated (due to hardware, stents, pacemakers, etc.), MDCT has a lot to offer beyond bone."
By Eric Barnes
AuntMinnie.com staff writer
June 20, 2005
Related Reading
MRI sees spinal metastases earlier, but low-dose whole-body MDCT aces skeletal workup, May 20, 2005
Cryoablation provides effect palliation for bone metastasis, April 4, 2005
MDCT staging may obviate bone scintigraphy in some patients, March 6, 2005
Copyright © 2005 AuntMinnie.com