TORONTO - The use of cognitive behavior therapy (CBT), the application of cognitive psychotherapy to change thinking patterns combined with behavior therapy to modify the connections between situation and reaction, in patients with bulimia nervosa results in increased mu-opioid receptor (mu-OR) binding, according to a presentation Sunday at the Society of Nuclear Medicine (SNM) meeting.
Bulimia is generally considered to be a psychological and emotional disorder, which sometimes coexists with other psychiatric disorders, such as depression or obsessive-compulsive disorder. The condition is marked by recurrent instances of binge eating followed by recurrent inappropriate compensatory behavior to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, enemas, or other medications; fasting; or excessive exercise.
A research team from the departments of radiology and psychiatry at the Johns Hopkins University School of Medicine in Baltimore compared mu-OR binding in bulimia nervosa patients before and after CBT, as well as in a healthy control group.
"Our objective was to investigate the relationship between change in mu-opioid receptors binding and bulimic behavior frequencies before and after 12 weeks of CBT," said Dr. Badreddine Bencherif, who presented the results of the group's research.
The team conducted PET scans on 13 females (11 Caucasian, one African-American, and one Asian; mean age, 26) with bulimia nervosa and on eight healthy females (all Caucasian, mean age 25). 11C-carfentanil, a synthetic highly specific mu-OR agonist, was used to measure brain mu-OR binding in the study group.
The dynamic acquisition scans were conducted on a GE Healthcare (Chalfont St. Giles, U.K.) Advance PET system over a period of 90 minutes postinjection of 20 (±2) mCi of 11C-carfentanil. A thermoplastic mask individually fitted to each subject's face was used for immobilization and structural localization during PET acquisition, Bencherif said.
The control group was imaged once, while the bulimia nervosa group was imaged before and after CBT. Data on change in cognitive symptoms and bulimic behavioral frequencies between the PET scans were correlated with changes in mu-OR binding. According to Bencherif, parameterized images for 11C- carfentanil PET were generated on the basis of a Logan graphical analysis with a reference-tissue, occipital lobe, input function. The scan data and parametric images were then processed utilizing statistical parametric mapping.
Eight of the BN patients responded positively to CBT, and the other five had a partial response to psychotherapy.
"A partial response was considered if a subject had more than four days of binging and vomiting behavior within a two-week period," Bencherif said.
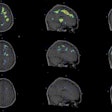
The analyses of the bulimia nervosa patients' images demonstrated changes in mu-OR binding in the prefrontal cortex, left inferior temporal regions, left insula, and cingulate cortex. Prior to CBT, mu-OR binding showed a decrease in the prefrontal cortex, cingulate cortex, and insula in the bulimia nervosa patients when compared with the control group.
Post-treatment with CBT, the bulimia nervosa group that responded positively to therapy showed increased mu-OR binding in these areas. The partial responders still demonstrated decreased receptor binding, Bencherif noted.
According to the researchers, the change in binge behavior frequency correlated negatively with receptors binding in cingulate cortex, whereas decreased preoccupation with food and decrease in vomiting urges following treatment both correlated positively with a decrease in mu-OR binding in the prefrontal cortex and insula.
They believe that the change in opioid receptors in response to CBT suggests a state rather than trait relationship between mu-OR binding and bulimic behavior. The research suggests that PET imaging could be helpful in matching bulimia nervosa patients to treatment options.
"A higher baseline mu-opioid binding in the insula and prefrontal cortex seems to predict a better outcome to cognitive behavior therapy," Bencherif said. "However, we need to conduct similar studies across a larger patient population."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
June 20, 2005
Related Reading
Racial profiling: fMRI links brain activity and black-white bias, May 27, 2005
Neuroimaging study bolsters genetic basis for feeling down, May 19, 2005
fMRI identifies link between alleles, amygdala in affective disorders, March 22, 2005
MRSI may be just the "tool" to diagnose bipolar disorder, November 30, 2004
Sexual healing: Imaging takes a roll in the hay with human relations, April 29, 2004
Copyright © 2005 AuntMinnie.com