Move over angiography. A study to be published this week in the Journal of the American Medical Association concludes that multidetector-row CT angiography, while not a fully developed technology, is a highly accurate complement to invasive coronary angiography. And although spatial limitations are still an issue with 16-slice CT scanners, CTA avoids several potential risks associated with invasive x-ray angiography.
These findings won't surprise radiologists who are familiar with the impressive cardiac imaging capabilities of 16-slice CT scanners. A few have experienced even better results with 40- and 64-slice machines that are just now being incorporated into practices.
Still, the study's direct comparison of angiography and CTA in its entire patient cohort (also aided, perhaps, by its publication in JAMA's prestigious pages) could exert a warming effect on the glacial pace of change in the practice of cardiac disease assessment. So while conventional angiography remains the diagnostic standard for clinical evaluation of known or suspected coronary artery disease (CAD), the authors concluded that it may not always be thus.
"The risk of (angiography-related) adverse events is small, but serious and potentially life-threatening sequelae may occur, including arrhythmia, stroke, coronary artery dissection, and access site bleeding (total complication rate 1.8%; mortality rate 0.1%)," wrote the authors Drs. Martin Hoffmann, Heshui Shi, Bernd Schmitz, Florian Schmid, and colleagues from the University of Ulm in Germany. "Furthermore, catheterization induces some discomfort and mandates routine follow-up care (JAMA, May 25, 2005, Vol. 293:20, pp. 2471-2478).
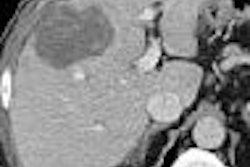
Hoffman et al assessed the diagnostic accuracy of 16-slice MDCT versus invasive coronary angiography in 103 patients (average age 61.5 years) with known or suspected CAD. MDCT and conventional angiography were performed a mean of 16.3 days apart.
A scout acquisition and CTA images were acquired on the MDCT scanner (Brilliance, Philips Medical Systems, Andover, MA), preceded by administration of 1.2 mL/kg of iodinated contrast followed by a 50-mL saline flush, with a test bolus used to determine flow rate (mean 4 mL/sec). Collimation was at 16 x 0.75 mm, pitch was variable between 0.2 (heart rate < 65 bpm) and 0.3 (heart rate > 75), rotation time was 0.42 msec, with tube current of 120 kVp and mAs of 180-300 depending on heart rate. Metropolol (up to 20 mg) was administered in patients with resting heart rates of 75 bpm or greater.
Prospectively triggered tube-current modulation was used to acquire images in mid-diastole (75% of the R-R at 5% intervals), with a radiation dose of approximately 4.9 mSv, depending on heart rate. The mean and standard deviation heart rates were 68.7/min and 11.6/min, respectively (range 45-111 min). Prospectively triggered tube-current modulation was applied in 46 patients.
The observers used a smooth-tissue filter kernel for reconstruction, choosing the best cardiac reconstruction phase in a side-by-side comparison. Each segment was evaluated for image quality and artifacts caused by motion, partial-volume averaging, poor contrast opacification, and high-density objects, the authors wrote.
Conventional angiograms were read by two readers blinded to the results of MDCT imaging, with coronary arteries divided into segments based on American Heart Association guidelines. Stenosis, expressed as the percentage of lumen reduction, was measured using QCAPlus version 0.310.30 software (Sanders Data Systems, Palo Alto, CA).
Twenty-five patients were excluded, leaving a total of 103 patients or 1,384 total segments to evaluate. MDCT was nondiagnostic in only 88 (6.4%) of these cases, consistent with previous studies and due mainly to faster heart rates, according to the study team. Compared to angiography for detecting stenotic lesions 50% and greater, MDCT had a segment-based sensitivity of 95%, specificity of 98%, positive predictive value of 87%, and negative predictive value of 99%.
"Multislice CT correctly identified 38 of the 45 patients (84%) without significant stenosis demonstrated by conventional invasive angiography," the authors wrote. "Two of 58 patients with CAD were not detected by (MDCT)." These included a proximal lesion in the posterior descending artery and one diagonal branch lesion missed due to inadequate opacification. "Patients with single-vessel disease demonstrated by invasive coronary angiography (n = 22) were either correctly classified (n = 15, 68%) by (MDCT) or were misclassified as having multivessel disease (n = 5, 23%)," they stated.
In addition, the quantitative comparison of stenosis grading between MDCT and angiography showed comparable correlation (r = 0.87, p < 0.001), and CT measured a greater percentage of stenoses (bias +12%; limits of agreement -19% to +43%), according to a Bland-Altman analysis.
The area under the curve for identifying patients with stenoses eligible for recatheterization was 0.97 (95% CI, 0.91-1.00), and the confidence bounds widened slightly after excluding patients who had undergone percutaneous coronary intervention (95% CI, 0.90-1.00).
The use of threshold optimization allowed either detection of stenoses with 100% sensitivity at a reasonable false-positive rate (specificity 76.5%; MDCT stenosis > 66%) or optimization of both sensitivity and specificity ( > 90%; MDCT stenosis > 66%).
"We found that, compared with invasive coronary angiography, (MDCT) has a high discriminative power to detect obstructive CAD," the authors wrote. "This is not only shown for the detection of the standard definition of significant disease, defined as greater than 50% lumen narrowing of the coronary artery, but also at other thresholds." And MDCT can easily distinguish patients who are candidates for revascularization, they added.
And because ROC analysis is independent of prevalence, the results seen in patients at moderate to high risk might well be applicable to lower-risk populations, making the MDCT approach feasible for screening lower-risk populations as well, they noted.
"Our findings are consistent with multiple single-center studies showing consistent high accuracy and negative predictive values," the team wrote. "The indication is limited by false-positive rates that consecutively reduce specificity and positive predictive value."
CTA results have improved significantly compared to earlier findings using four- and eight-detector scanners, but the segment-based exclusion rate of 6.4% still corresponds to incomplete coronary tree coverage in 27% of the patients. As a result, MDCT isn't ready yet to challenge coronary invasive angiography "as a true alternative," the authors wrote.
"Further improvements are needed for accurate delineation of the coronary lumen adjacent to high-density objects such as calcified plaque or stent struts," they wrote. But extrapolating the results to scanners with more detector rows, this shortcoming seems destined to be conquered.
In addition to more detectors, faster gantry rotation times and the use of beta blockers to reduce the number of poorly imaged segments can also make significant improvements.
Overall, MDCT demonstrated reasonably high accuracy for detecting significant stenosis when assessed at the patient level, which may be the only level that matters, the group concluded. At its current stage of development, MDCT can be used to substantially reduce the likelihood of clinically important coronary artery disease, while avoiding most of the risks associated with invasive coronary angiography.
By Eric Barnes
AuntMinnie.com staff writer
May 24, 2005
Related Reading
Noncoronary findings often identified on CT coronary angiography, May 18, 2005
Scores of detector rows bring opportunities, challenges to CT imaging, April 8, 2005
RV function scans integrated with chest CT, May 9, 2005
New study to assess 64-slice coronary CTA, March 22, 2005
High-concentration iodine quickly opacifies pig arteries, March 10, 2005
Copyright © 2005 AuntMinnie.com