CT enteroclysis is proving to be a fast, accurate, and relatively easy alternative to x-ray enteroclysis, fluoroscopic barium small-bowel follow-through (SBFT), and other small-bowel exams.
A just-published study of 107 patients in France found that multidetector-row CT enteroclysis was well-tolerated and highly sensitive for the detection of small-bowel masses, Crohn's disease, and low-grade obstructions of the small bowel (Radiology, November 2004, Vol. 233:2, pp. 338-344).
Studies to be unveiled at this year's RSNA show in Chicago show similarly high sensitivities in the high 80% range, though CT, like SBFT, yields its share of false-positives and false-negatives (RSNA listings include 1923GI-p, 1974GI-e, and SSQ06).
Dr. C. Daniel Johnson from the Mayo Clinic in Rochester, MN, recently said that his group has begun recommending CT enteroclysis (Mayo calls the exam "CT enterography" or "CTE") as the front-line imaging exam in patients with suspected small-bowel disease, relagating SBFT to a lesser role as a problem-solving tool. Johnson made his remarks at the 2004 International Congress of Radiology in Montreal.
Paris performance
"Although (x-ray) enteroclysis has a high sensitivity for facilitating the diagnosis of most small-bowel abnormalities, this technique has limitations, including high radiation dose and indirect information about the status of the bowel wall and adjacent structures," Drs. Mourad Boudiaf, Ameer Jaff, Philippe Soyer, and colleagues from Hôpital Lariboisière-AP-HP in Paris wrote in Radiology.
 |
| All images are of a 21-year-old woman who presented with symptoms typical of Crohn's disease: recurrent episodes of hemorrhagic diarrhea, abdominal pain, weight loss, and fever. Endoscopy showed segmental changes in the colon and the terminal ileum; histopathology showed granulomatous mucosal inflammation. In image above, normal enteroclysma CT, coronary reconstruction, shows optimal distension of small-bowel loops. All images courtesy of Dr. Johannes Sailer and Dr. Philipp Peloschek, Department of Radiology, Medical University of Vienna. The group will present its CT enteroclysis results later this month at RSNA scientific presentation presentation No. SSQ06-06). |
The French researchers used CT enteroclysis to examine 107 patients suspected of having a small bowel tumor (n = 8), active inflammatory disease (n = 18), unexplained gastrointestinal bleeding (n = 36), refractory celiac sprue (n = 14), or a low-grade small-bowel obstruction (n = 31).
A nasoenteric tube (8-F) was inserted into the duodenojejunal junction under fluoroscopic guidance in each patient. The small bowel was distended with water (up to 2,000 mL) using a pressure-controlled pump. Before CT imaging, the patients also received 120 mL of iodinated contrast material (70-second delay), and 10 mg of the antispasmodic drug tiemonium methylsulphate (Viscéralgine, Laboratoires Cerm, Puteaux, France).
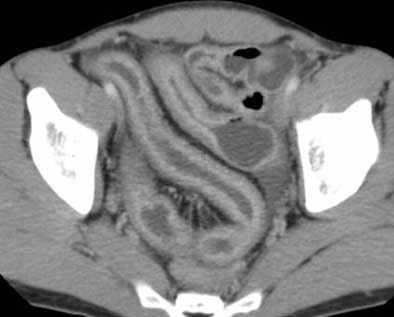 |
| Top and below: In same 21-year-old patient, axial CT enteroclysis shows long-segment inflammatory reaction and severe thickening of the terminal and preterminal ileum due to histologically proven Crohn's disease. Bottom image, equivalent coronal multiplanar reformation. |
 |
 |
MDCT images were acquired using 4 x 2.5-mm collimation on a Plus 4 Volume Zoom scanner (Siemens Medical Solutions, Erlangen, Germany) using 120 kVp, 165 mAs, and table speed of 12.5 mm per rotation, and reconstructed at 3-mm intervals using a soft-tissue algorithm on a Siemens Volume Wizard workstation.
"Reformatted images were routinely obtained in the coronal plane," the authors wrote. "To best analyze bowel loops, the radiologist who performed the examination created additional reformatted images in the sagittal and oblique planes by manually tracing a ray along the abnormal small-bowel loop." Two experienced gastrointestinal radiologists, blinded to the results of concurrent barium and endoscopic studies, examined the images in two separate reading sessions.
 |
| Conventional enteroclysis of the same patient shows inflammatory contour irregularities of the mucosal relief in the region of the Bauhini's valve and the terminal ileum; presence of a fistula was suspected. Additionally, there is a stenosis of the preterminal ileum with dilatation of the prestenotic loop. |
As for the reference standard, 90/107 patients had invasive exams such as push enteroscopy, endoscopy, videocapsule endoscopy, and/or histology comprised the reference standard; 17 had other imaging studies or clinical follow-up. Still, the use of multiple reference standards was seen as a limitation.
The exam was well-tolerated in 106 patients; one complained of abdominal pain after the exam, the authors wrote, noting that nasojejunal intubation was also well-tolerated. Optimal small-bowel distension was achieved in 70% of the patients, though two patients had suboptimal distension in the distal portion of the ileum.
MDCT found 21 small-bowel masses (including four carcinoid tumors 5-20 mm depicted as focal nodular lesions), and nine cases of active Crohn's disease.
"In all cases of Crohn's disease, CT enteroclysis accurately demonstrated the mural and extramural inflammatory changes," the group noted.
"All pertinent information leading to the final diagnosis was depicted on transverse CT enteroclysis images," they wrote. "Multiplanar reformatted CT enteroclysis images did not provide any additional information."
CT also found small-bowel tuberculosis in two patients, and small-bowel lymphoma complicating celiac disease in four. CT also confirmed low-grade bowel obstruction in 12 patients. Compared to the reference standard exams, CT's reported sensitivity, specificity, positive predictive value, and negative predictive value were 100%, 95%, 94%, and 100%, respectively.
SBFT failed to demonstrate nine tumors, including lymphoma in one patient and one case of ulcerative jejunoileitis. Enteroscopy (eight patients) missed seven tumors, including one lymphoma and two cases of ulcerative jejunoileitis "because the disease was located far away from the duodenojejunal junction or far from the ileocecal valve," they wrote. CT had three false-positive findings, due to a transient intussusception, a pseudotumor (thickened fold), and suspected angiodysplasia that was not confirmed by endoscopy.
And in a strength CT is known for, unsuspected extradigestive disease was found in six patients. The cases included metastatic lymph nodes (n = 2), and association of liver metastases and metastatic lymph nodes (n = 4).
"CT enterography proved more informative than barium studies and endoscopy," they concluded. "Our results suggest that CT enteroclysis could replace the combination of abdominopelvic CT study and barium follow-through examination that is commonly performed for the evaluation of patients with small-bowel tumors, thus decreasing the patient's exposure to ionizing radiation," the authors wrote.
Mayo experience
The fluoroscopic SBFT exam has performed well at the Mayo Clinic for years, Dr. C. Daniel Johnson told attendees at the 2004 International Congress of Radiology in June.
The problem is that while SBFT can reliably demonstrate early mucosal disease, including aphthous and linear ulcers, the radiologist must rely on nonspecific secondary signs to evaluate the small-bowel wall and mesentery. The group is reluctant to replace the fluoroscopic exam, Johnson said, but SBFT has important limitations that CT enterography is often able to overcome.
"The limitations of SBFT are really the driving force behind the change," said Johnson, who is a professor at Mayo Medical School and a radiologist at Mayo Medical Clinic. "Many bowel loops can be overlapping and obscure pathology. Particularly, patients that have lots of pelvic loops can be difficult to really assess, and many times you feel ... you didn't get as good a look at the small-bowel loops as you would have liked to."
On the other hand, well-performed CT enterography can reliably depict the entire small-bowel lumen. It enables the radiologist to assess bowel-wall thickness, as well as the mucosal enhancement and lesions associated with inflammatory conditions such as Crohn's disease. Last but not least, important extragastric abnormalities have been found with CTE, he said.
Feasibility study
Johnson also outlined a feasibility study the group published last year that involved 23 patients with known or suspected active Crohn's disease in the terminal ileum (Radiology, October 2003, Vol. 229:1, pp. 275-281).
In the study, Drs. Peter Wold, Joel Fletcher, Johnson, and colleagues aimed to compare CT enterography with SBFT, while looking for distension differences, if any, between water taken orally and a methylcellulose solution delivered via nasojejunal tube. In all, eight patients had a 13-F gastroduodenal tube and methylcellulose (1,800 mL injected at 60 mL/min), while 15 drank water (1,800 mL in 450-mL aliquots over 75 minutes). The reviewers subjectively ranked the quality of luminal distension on a scale of 1 (less than 40% adequate distension) to 4 (more than 90%).
Both groups underwent CTE and SBFT (as well as colonoscopy and ileoscopy), with endoscopy and histology used as reference standards, Johnson said. Ten mg of metoclopramide (Reglan, Pharmaceutical Associates, Greenville, SC) was administered as a first step, 75 minutes prior to imaging to promote bowel filling, and 1 mg of IV glucagon was administered as an antispasmodic.
MDCT portal venous-phase and arterial-phase images were acquired following administration of 150 mL iopamidol (Isovue 300, Bracco Diagnostics, Princeton, NJ) on a LightSpeed or LightSpeed Plus scanner (GE Healthcare, Waukesha, WI) using 2.5-mm collimation, 270 mAs, 120 kVp, and reconstructed at 2.5 mm.
Based on a review of all data, 20/23 patients received a final diagnosis of Crohn's disease, two were diagnosed with ulcerative colitis, and one was said to have chronic abdominal pain of unknown etiology.
Oral contrast
Luminal distension did not differ significantly (p = 0.16) between the peroral water (mean distension score 2.10) and the intubated methylcellulose patients (mean distension score 2.75), though there was a trend toward better jejunal distension in the latter.
"This seems to be the biggest bugaboo for us -- trying to get the jejunum reliably distended in every patient," Johnson said. "Sometimes you can -- sometimes it's pretty flat.... I think the (nasogastric) tube really gives us an edge for good evaluation of the jejunum."
And just since the summer, a new low-attenuation oral contrast agent, VoLumen (E-Z-EM, Lake Success, NY) seems to be outperforming both water and methylcellulose, he said. These days, all patients are receiving 1,500 mL of the sorbitol-and-gum-based mixture before CTE.
The peroral CTE protocol yielded two false-negative findings in two patients, and fluoroscopy was also deemed normal, while endoscopy showed a solitary aphthous ulcer in the terminal ileum. CTE was also false-negative in a patient with multiple aphthous erosions in the neoterminal ileum. Two active Crohn's disease patients were seen at CTE but not SFBT.
The noninvasive peroral water protocol detected active Crohn's disease in 12/15 cases (80%) versus 7/8 (88%) for the nasojejunal tube technique, versus 17/23 (74%) for SBFT, the group reported in Radiology.
Extraintestinal findings
In all, CTE demonstrated active Crohn's disease in 10/13 patients, based on mucosal hyperenhancement in nine, mural stratification in five, or mesenteric fat stranding in four patients. SBFT detected active terminal ileal Crohn's disease in 8/13 patients. Arterial-phase imaging did not contribute to the diagnosis in 22/23 patients, though the group had hypothesized that early phase images might demonstrate subtle mucosal enhancement. Still, CT may have difficulty depicting mild inflammation, the group reported.
CT's ability to detect active Crohn's disease is pretty exciting stuff, Johnson said in his presentation. "Sometimes you can see it with SBFT -- if you see the aphthous ulcers or complete ulceration of the mucosa -- but sometimes you can't be sure what the disease activity is."
A growing arsenal of powerful drugs on the market for Crohn's disease makes it increasingly important to know whether the patient has active disease, and is responding to therapy, Johnson said, a job for which CTE seems well suited with its ability to detect hyperenhancing lesions. "Look how bright the mucosal enhancement is in this patient with very active Crohn's disease," he said of a case study.
Next came images of patients with inactive disease (fat deposits in the ileum wall) and recurrent disease, also detected on CT. Extraintestinal abnormalities are icing on the cake, and were detected by CT in the gallbladder, kidney, and colon. Kidney and gallbladder stones are part of the Crohn's disease process, and radiologists should be looking for them, Johnson said.
"I was surprised by how often we saw the colon," he said. "By the time we got to the colon it was often filled with water, and we get a beautiful look at the hyperenhancing thickened wall in this patient that had Crohn's colitis."
The group is not giving up on SBFT -- it can demonstrate some abnormalities that CT misses -- but CT offers so much information that it should be the first-line exam, Johnson said. "CT's ability to detect treatment response in patients with active Crohn's disease, and its ability to detect significant extraintestinal findings also bode well for the exam," he said. And compared with fluoroscopy, CT is faster.
"For young patients that have Crohn's disease, the scheduling advantage (for CT) is huge," Johnson said. "Our internists love it for this reason alone. Our patients can come in, have the CT exam in the morning, colonoscopy in the afternoon after removal of fluid, and they can go home. These are people with young families, they may not have good insurance, and they need to get back to work quickly. (With SBFT) it took another day to get the barium out."
By Eric Barnes
AuntMinnie.com staff writer
November 18, 2004
Related Reading
Survey finds most small-bowel exams are substandard, April 16, 2004
Capsule endoscopy fares well in small bowel versus CT, barium enema, January 14, 2004
Post-toilet cystoproctography pinpoints enteroceles of small bowel, May 9, 2003
Dynamic MR enteroclysis negotiates twists, turns of small bowel disease, February 5, 2003
Copyright © 2004 AuntMinnie.com