As they refine coronary calcium assessment techniques, some radiologists are putting more emphasis on the atherosclerotic disease process, in hopes of gaining a more nuanced understanding of coronary calcium’s role in atherosclerosis and its proper place among other markers of cardiovascular disease.
Among the key questions: when is CT calcium screening most clearly indicated, and when might calcium assessment with CT be less informative? Are there combinations of disease risk and calcium score that require additional follow-up in asymptomatic patients? What is the role of heredity in the morbidity that results from atherosclerosis?
At the 2004 European Congress of Radiology in Vienna, investigators from Spain examined these questions in a study of 152 asymptomatic patients who were self-referred for cardiovascular disease risk.
"Currently it is widely accepted that atherosclerosis is an inflammatory disease," said Dr. Octavio Cosin from the University of Pamplona. "The presence of cardiovascular risk factors promotes the atherosclerotic process, which begins with a so-called endothelial dysfunction; the endothelium produces some properties and when they continue a tapestry will appear. This tapestry will show an intense inflammatory activity, with the presence of inflammatory cells that (boost) several markers of inflammation."
Later on, the atheroma is covered by a fibrous cap that can break, producing local thrombosis or even calcificate.
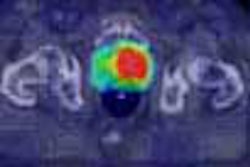
By gauging several markers of atherosclerotic disease, Cosin and colleagues hoped to gain a better understanding of calcium’s role as a risk factor. Specifically, they sought to correlate coronary calcium scoring risk categories with other methods of cardiovascular risk prediction, including traditional risk factors, C-reactive protein, fibrinogen, von Willebrand levels, and femoral and carotid intima-medial thickness.
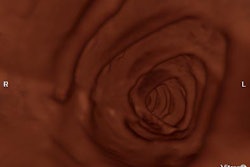
In the study, coronary calcium scoring was performed in 152 asymptomatic patients (141 males, 92.8%, ages 31-81), who underwent multidetector-row scanning on a Volume Zoom scanner (Siemens Medical Solutions, Erlangen, Germany) at 4 x 2.5-mm slice thickness, collimation 3 mm, table feed 3.5 mm, reconstruction interval 1.5 mm, and kernel B35f.
The patients were divided by their Agatston calcium score into very low risk (64 patients, score [mean + standard deviation] 0 ± 0), 25 low risk (3.3 ± 2.7), 32 at moderate risk (37.4 ± 22.5), 16 patients at moderate-high risk (203.9 ± 85.0) and 15 at high risk of coronary artery disease (1,178.2 ± 806.4). The group also underwent testing for a variety of other risk factors, including ultrasound measurements of intima-medial (IMT) thickness made by radiologists who were blinded to the other results.
"According to our first objective, we found poor correlation between calcium score and risk with most of the cardiovascular disease risk factors, chief among them intima-medial thickness," Cosin said. In addition to IMT, the Agatston score showed poor correlation with diastolic and mean blood pressure values, BMI, atherogenic lipoproteins, glucose blood levels, and fibrinogen (p>0.05).
However, "we found significant correlation (of Agatston score-based risk stratification) with histolic blood pressure, and CRP levels (p<0.05), and highly significant correlation with age and PROCAM (Prospective Cardiovascular Münster Study) risk equation factors (p<0.01)," Cosin said, noting that previous studies have also shown poor correlation between inflammatory markers such as fibrinogen.
"As for the question of when to initiate calcium scoring in an asymptomatic population, we found that if a person has a very low pretest cardiovascular risk, we most probably will find a low coronary calcium score," Cosin said. "On the other hand, if we have a patient that shows high risk, we still (lack) enough evidence to avoid intervention in these patients based only on a calcium score. But when it comes to the moderate-risk group, we found poor correlation (even) between PROCAM results and coronary calcium studies."
Among individuals, the clinical aptitude for CVD risk can be confounding, he said. For example, there were two patients in the study with similar age, and high blood pressure. Patient 2 had elevated cholesterol levels and was a smoker. PROCAM values showed patient 1 as zero risk, and patient 2 at 1.15, which is moderate risk.
But a coronary calcium scan showed dense calcification in patient 1 and no calcium in patient 2. "We think these patients should be treated differently," he said. He concluded that global risk profiles can be used to indicate coronary calcium studies in moderate-risk patients.
"With moderate (cardiovascular disease) risk, a coronary calcium study can finally be included as a definite risk factor in global risk equations," Cosin said. When assessing risk, it is also important to pay attention to genetics, which is responsible for 40% of the risk of cardiovascular disease.
"Due to genetics, patients with the same risk factors react differently, and the same coronary arteries react differently," Cosin said.
By Eric BarnesAuntMinnie.com staff writer
April 6, 2004
Related Reading
Perfusion defect patterns help spot stenoses in angina patients, March 29, 2004
Patients shape up after viewing CT scans of their own blocked arteries, March 24, 2004
Accuracy of multidetector CT for coronary stenosis depends on patient selection, March 15, 2004
Copyright © 2004 AuntMinnie.com