In light of radiology's fervent focus on coronary CT angiography (CTA), unstable coronary artery plaque, and the like, one might be forgiven for wondering if coronary artery calcium even matters anymore -- or whether it has simply fallen out of fashion.
Indeed, calcium still matters mightily, even in 2008, according to Dr. J. Jeffrey Carr, a professor of radiologic sciences at Wake Forest University in Winston-Salem, NC. At the 2008 International Symposium on Multidetector-Row CT in Las Vegas, Carr dedicated nine minutes to debunking "urban myths" about calcium that he hears from medical professionals who should know better.
Myth #1: Calcium is just a surrogate marker for coronary artery disease, isn't it? Is there an alligator in the New York City sewer system?
Calcified plaque is atheroma, technically an American Heart Association (AHA) type Vb atheroma that takes an individual from having risk factors for atherosclerosis to having documented disease, Carr said.
"Whether you're reading a noncontrast chest CT, an ungated CTA, or [using] a super-duper four-tube 800-channel system, if you identify little white dots along a coronary artery, you've identified someone that has advanced atheroma of coronary artery disease," he said.
Myth #2: Coronary calcium is just debris. It's just stable, burnt-out disease. What I really want to know about is this exciting unstable plaque -- that's what causes deaths, that's what I want to know, that's what my patients want to know. I don't care about coronary calcium!
But multiple studies say one should care. A 2004 study looked at 178 individuals using intravascular ultrasound (IVUS). Researchers were looking for the culprit lesion that had caused events such as acute myocardial infarction, unstable angina, and stable angina (Circulation, November 30, 2004, Vol. 110:22, pp. 3424-3429).
But what caused the problem "wasn't echogenic plaque, it wasn't the lipid core as you might think," Carr said. It was calcium.
Not only did the results show that the frequency of calcium deposits was significantly different in patients suffering events, the average number of calcium deposits within an arc of 90º was significantly higher in those with acute myocardial infarction (AMI) compared to those with stable angina (p < 0.0005).
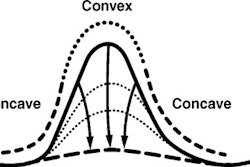
"In AMI patients, the typical pattern was spotty calcification, associated with a fibrofatty plaque and positive remodeling," Ehara and colleagues reported.
"Really, the idea of vulnerable plaque is falling by the wayside, and we really want to think about vulnerable patients and vulnerable segments of vessels," Carr said. "So when you see a spotty pattern of calcification, what we're seeing is a segment of the artery that has mixed and complex lesions in it," which in this study consistently identified the culprit lesion.
Myth #3: The presence of coronary artery calcium is somewhat static and stable.
In a 2007 study published by the Woman's Health Initiative, 1,064 women (mean age 55 years) were randomized to receive estrogen hormone replacement therapy (HRT) or a placebo for a mean 7.4 years of treatment. HRT had a protective effect. The researchers found a 42% reduction in calcified plaque among women randomized to receive HRT and a 61% reduction in plaque in those with at least 80% adherence to the study medication (New England Journal of Medicine, June 21, 2007, Vol. 356:25, pp. 2591-2602).
"For this relatively short period of time, you're seeing how HRT dramatically reduced the burden of plaque in the coronary arteries," Carr said.
Myth #4: Everyone gets calcified plaque -- can't we just ignore it in old people?
Apparently not. The Rotterdam Coronary Calcification study followed 1,795 older asymptomatic individuals for a mean 3.3 years (mean age, 71 years; range, 62 to 85 years) seeking to correlate the incidence of cardiac events with the presence of coronary artery calcification at electron beam CT (Circulation, July 26, 2005, Vol. 112:4, pp. 572-577).
Vliegenthart and colleagues reported that the relative risk of coronary events was 3.1% (95% confidence index [CI], 1.2 to 7.9) for calcium scores of 101 to 400, 4.6% (95% CI, 1.8 to 11.8) for calcium scores of 401 to 1000, and 8.3% (95% CI, 3.3 to 21.1) for calcium scores greater than 1000 compared with calcium scores of 0 to 100.
The study showed a strong correlation between coronary artery calcium, events, and survival even in the elderly, Carr said -- and in short order. "We're not talking decades here. We're talking four years," he said.
Myth #5: Atherosclerosis and coronary artery disease is a condition of middle-age and older adults.
This is probably the most troubling myth, according to Carr. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study researchers performed autopsy examinations of the left anterior descending (LAD) artery of younger individuals (mean age, 33) who had died in accidents, homicides, and suicides (Circulation, July 25, 2000, Vol. 102:4, pp. 374-379).
Approximately 19% of 30- to 34-year-old men and 8% of 30- to 34-year-old women had atherosclerotic stenosis ± 40% in the LAD, McGill and colleagues reported.
"What's really scary is if you look at 15- to 19 year-old men, 4% had 40% LAD lesions," Carr said. "So we need to realize that atherosclerosis and coronary artery disease is a pediatric condition. If we're going to change the dynamics, we're going to need to change our concept of the disease to one of children, teenagers, and young adults."
The results are supported by recent data from the Coronary Artery Risk Development in Young Adults (CARDIA) study. In individuals with a mean age of 45 years (range, 38 to 50 years), 19% had advanced atheromatous coronary artery disease, Carr said (Arteriosclerosis, Thrombosis, and Vascular Biology, January 1991, Vol. 17:1, pp. 51-55).
Myth #6: Coronary calcium doesn't work in women and minorities. Show me data that it adds to traditional risk factors such as the Framingham risk score in someone besides white men who we already know are at high risk.
The recently published Multi-Ethnic Study of Atherosclerosis (MESA) assessed calcium as a predictor of coronary events in four ethnic groups: whites (38.6%), blacks (27.6%), Chinese Americans (11.9%), and Hispanics (21.9%) (New England Journal of Medicine, March 27, 2008, Vol. 358:13, pp. 1336-1345).
Compared to those with no coronary calcium, the adjusted risk of a coronary event was increased by 7.73% among participants with calcium scores between 101 and 300, and by 9.67% among those with scores above 300 (p < 0.001 for both comparisons), Detrano and colleagues reported.
Among the four racial and ethnic groups, a doubling of the calcium score increased the risk of a major coronary event by 15% to 35% and increased the risk of any coronary events by 18% to 39%, the authors reported.
In addition, the areas under the ROC curves for predicting major coronary events and any coronary event were higher when the calcium score was added to the standard risk factors, the group wrote.
"This is the area of curve that shows that coronary calcium added to the Framingham score increases risk substantially -- applying additional information beyond traditional risk factors," Carr said.
Myth #7: With coronary CTA, who needs calcium scoring anymore?
It's a matter of perspective -- and taking the time to do calcium scoring for the benefit of the patient, Carr said.
He gave an example of a 50-year-old woman presenting with chest pain and a low-risk thrombolysis in myocardial infarction (TIMI) score of 1. Coronary CTA showed minor coronary artery calcifications.
Lacking a calcium score, report option #1 concludes that the patient had nonobstructive coronary artery disease (CAD) and recommends "healthy lifestyle and additional cardiovascular disease prevention as appropriate."
But the risk picture becomes clearer when the calcium score is calculated. Thus, report option #2 reads:
"Nonobstructive CAD present. Calcium score 130, > 99th percentile plaque burden for age, gender, and race with a seven- to tenfold increase in hard events (myocardial infarction and death) over the next four years. Recommend health lifestyle and cardiovascular disease prevention as appropriate."
If the practice routinely calculates the calcium score, producing report option #2, no further risk assessment will be needed, Carr said. So is coronary calcium still worth measuring in this day and age?
"Calcified plaque documents the presence of coronary artery disease," Carr said. Coronary calcified plaque predicts hard coronary artery and cardiovascular disease events in men, women, and minorities. "The calcium score adds significantly to risk prediction of near-term events, and calcium score has an important role even in the age of coronary CT angiography."
By Eric Barnes
AuntMinnie.com staff writer
May 26, 2008
Related Reading
Incidental findings on cardiac MDCT common for healthy adults, May 9, 2008
Coronary calcification increases likelihood of aspirin and statin usage, April 10, 2008
Cardiac CT saves money and time as first-line heart test, April 1, 2008
Coronary calcium score predicts coronary events in 4 major ethnic groups, March 28, 2008
Coronary artery calcium suggests abnormal myocardial perfusion, February 12, 2008
Copyright © 2008 AuntMinnie.com