The worlds of radiology and high fashion don’t come together very often, but in late September they met head on: Avant garde New York designer Betsey Johnson was rushed to the hospital when an implant in her left breast ruptured. Upon further examination, clinicians determined that Johnson had breast cancer (Newsweek, October 2, 2000).
As the general population ages, and women who had implants put in nearly 20 years ago become candidates for regular breast screening, situations like Johnson’s may become more common. Despite controversy surrounding the procedure, the number of women who decide to have breast augmentation continues to grow. According to the American Academy of Cosmetic Surgeons, more than a quarter of a million women in the U.S. underwent breast augmentation in 1999.
A presentation at the Breast Imaging Conference last month in New Orleans focused on techniques for imaging the augmented breast. In addition, a multidisciplinary team of researchers used MRI to assess the prevalence of rupture in silicone gel implants in the American Journal of Roentgenology .
The nuances of augmentation
Radiologic technologist Rita Heinlein from the University of Baltimore in Maryland, along with radiologist Dr. Barbara Monsees of the Mallinckrodt Institute of Radiology in St. Louis, led the New Orleans workshop on imaging the augmented breast. Heinlein also presented a live demonstration on conducting mammography exams on these patients.
"For awhile, I think the number of women who chose to have implants declined when the controversy with silicone was going on," Heinlein said. "But with saline implants available now, I think more people are looking again at getting implants. It’s important to know some of the nuances of imaging implants."
The goal for imaging implants is to improve the amount of breast tissue that will be seen, Heinlein stated.
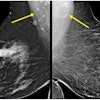
In the live demonstration, Heinlein outlined the five basic steps for imaging implants, as set out by the American College of Radiology. Two sets of views must be taken: one that includes the implant and one with the implant displaced.
"The full view with the implant in place is going to show us the deep tissue, whereas the displaced views are not. The full views allow us to look for implant rupture, " Monsees explained. "The displaced views…show the breast and parenchyma to its best advantage."
Getting the full view means using compression, but not so much to thin out the breast as to stabilize it.
"Don’t forget that the average compressed thickness of the average non-implanted breast is 4.5 cm or so. The average implanted breast is 7 cm, so there is a thickness difference. Many women are thicker than that. It depends on how compressible the implant is," Monsees said. "So you’ll start with a higher kVp -- I usually start with about 28 -- and you are aiming to see the interface between the silicone, or saline, and the tissue. Use just enough compression to prevent motion and motion-on-sharpness."
CC view
Heinlein began the demonstration with her technique for taking craniocaudal views.
1,2, 3
Copyright © 2000 AuntMinnie.com
As the general population ages, and women who had implants put in nearly 20 years ago become candidates for regular breast screening, situations like Johnson’s may become more common. Despite controversy surrounding the procedure, the number of women who decide to have breast augmentation continues to grow. According to the American Academy of Cosmetic Surgeons, more than a quarter of a million women in the U.S. underwent breast augmentation in 1999.
A presentation at the Breast Imaging Conference last month in New Orleans focused on techniques for imaging the augmented breast. In addition, a multidisciplinary team of researchers used MRI to assess the prevalence of rupture in silicone gel implants in the American Journal of Roentgenology .
The nuances of augmentation
Radiologic technologist Rita Heinlein from the University of Baltimore in Maryland, along with radiologist Dr. Barbara Monsees of the Mallinckrodt Institute of Radiology in St. Louis, led the New Orleans workshop on imaging the augmented breast. Heinlein also presented a live demonstration on conducting mammography exams on these patients.
"For awhile, I think the number of women who chose to have implants declined when the controversy with silicone was going on," Heinlein said. "But with saline implants available now, I think more people are looking again at getting implants. It’s important to know some of the nuances of imaging implants."
The goal for imaging implants is to improve the amount of breast tissue that will be seen, Heinlein stated.
In the live demonstration, Heinlein outlined the five basic steps for imaging implants, as set out by the American College of Radiology. Two sets of views must be taken: one that includes the implant and one with the implant displaced.
"The full view with the implant in place is going to show us the deep tissue, whereas the displaced views are not. The full views allow us to look for implant rupture, " Monsees explained. "The displaced views…show the breast and parenchyma to its best advantage."
Getting the full view means using compression, but not so much to thin out the breast as to stabilize it.
"Don’t forget that the average compressed thickness of the average non-implanted breast is 4.5 cm or so. The average implanted breast is 7 cm, so there is a thickness difference. Many women are thicker than that. It depends on how compressible the implant is," Monsees said. "So you’ll start with a higher kVp -- I usually start with about 28 -- and you are aiming to see the interface between the silicone, or saline, and the tissue. Use just enough compression to prevent motion and motion-on-sharpness."
CC view
Heinlein began the demonstration with her technique for taking craniocaudal views.
- Ask the patient to bend over from the waist so that the thorax is parallel to the ground. "The reason for that is to separate the breast from the implant so that I can have gravity to my advantage," Heinlein said. "That way I can easily pull this breast tissue away from the implant."
- Once the patient is bent over, ask her to take her hand and place it underneath the opposite breast, flat against the ribs. The RT can then either start at the nipple and push the implant back, or by placing the fingers on the ribs and the thumbs above, slide forward so that the implant moves back. "When I bring her up, the problem is that there will be a gap between the chest wall, the bucky, and her ribs," Heinlein said. "For that reason, you ask the patient to put her hand underneath the breast in order to fill that gap."
- The RT should place the edge of his or her fingers and hold the inferior tissue on the edge of the bucky.
- "What you are going to say to the woman is ‘I want you to push your body against your hand and you’ll see how the [top] bulges up.’ What I’m asking her to do is use the chest wall against the bucky to displace the implant more posteriorly. With this displaced, I can pull more tissue forward," Heinlein said.
- Using one hand to hold the implant back, place the other hand against the patient’s back. "This is key," she said. "You have to make sure that you are holding [the woman] in place because she is going to try to slide back from the bucky and you are going to lose some of that breast." Another option is to use a spatula against the displaced implant and flip it vertically to hold the implant back. Apply compression and remove the spatula.
1,2, 3
Copyright © 2000 AuntMinnie.com