Pulmonary Artery Sarcoma:
Clinical:
Pulmonary artery sarcoma is a very rare tumor. The majority of
patients with pulmonary
artery sarcomas present between the ages of 45-55 years, and there
is
roughly equal sex
distribution (although others report a 2:1 female predominence [2]
and others a slightly higher incidence in men (60%) versus women
(40%) [4]. The average age at diagnosis is 53 years [4].
Patients most commonly complain of symptoms related to acute or
chronic pulmonary hypertension with dyspnea (72%), chest pain
(45%), cough (42%), hemoptysis (24%), and
weight loss. The most
common finding on physical exam is a systolic ejection murmur
(44%) and
ECG demonstrates
evidence of right ventricular hypertrophy in about 40% of cases.
The
most common site of
metastases is the lung [2].
The median survival for untreated PAS has been reported to be as
low as 1.5 months and 10 months if surgical resection is performed
[4]. Overall
prognosis is very poor with a five year survival between 0 to
6% (median survival 14-27 months [4]).
Surgical treatment can be either pulmonary endarterectomy (most commonly), pneumonectomy or full thickness resection of the tumor from the vessel with vascular reconstruction using a Dacron graft [4]. Surgery, with or without adjuvant chemo/radiation therapy does improve short term survival.
X-ray:
The most common finding on plain film is hilar/pulmonary artery enlargement (53%) with decreased pulmonary vascularity (18%). Multiple pulmonary nodules are detected in 40% of cases.
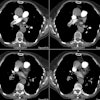
On CT or MR, the lesion appears as an intra-lumenal filling
defect
which typically occupies the entire lumen and expands the
vessel. The lesion generally arises from the intimal layer
of the
right, left, or main
pulmonary artery and extends as a polypoid lesion into the small
pulmonary arteries [2].
Less commonly the lesion grows in a retrograde fashion to involve
the
pulmonary valve and
right ventricle [2]. The "wall eclipsing" sign describes the
tendency of the lesion to "eclipse" or extend across the entire
cross-section of the vessel [4]. Direct transmural spread into the
adjacent lung,
bronchial wall, or
lymph nodes occurs in about 50% of cases.
Although the mass may appear
similar to
thrombus, findings which favor the diagnosis of sarcoma include
the
lack of other thrombi
and internal necrosis or ossification. Most lesions demonstrate
little or no enhancement at CT and can appear similar in
attenuation to bland thrombus [4]. Contrast enhancement can best
be
seen on post
gadolinium MR images and is typically heterogeneous, variable, and
often subtle requiring careful inspection of the contrast-enhanced
sequences [4].
Nuclear medicine: The lesion has been reported to show increased
FDG uptake in up to 90% of case [3,4].
Echocardiography will fail to detect about 75% of the lesions.
REFERENCES:
(1) J Comput Assist Tomogr 1997; 21 (5): 750-755
(2) AJR 2002; Dennie CJ, et al. Intimal sarcoma of the pulmonary arteries seen as a mosaic pattern of lung attenuation on high-resolution CT. 178: 1208-1210
(3) AJR 2007; Chong S, et al. Pulmonary artery sarcoma mimicking
pulmonary thromboembolism: integrated PET/CT. 188: 1691-1693
(4) Radiographics 2021; Ropp AM, et al. Intimal sarcoma of the
great vessels. 41: 361-379