Trapped Lung
Clinical:
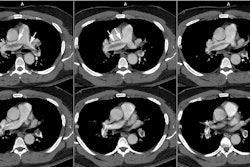
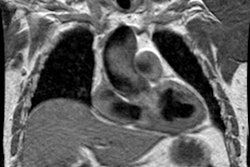
Trapped lung is a clinical entity characterized by the presence of a restrictive non-inflammatory visceral pleural peel [1]. The majority of affected patients are asymptomatic or have minimal dyspnea with exertion [1]. Following thoracentesis findings that suggest trapped lung include development of an unexpected pneumothorax, inability to fully expand the lung (with no history of current malignancy or infection), and inability to completely drain the effusion due to development of chest pain [1]. Etiologies include prior coronary bypass surgery, uremia, thoracic radiation, prior empyema, prior hemothorax, and repeated thoracentesis [1]. The pleural fluid is pauci-cellular with a mononuclear cell predominance [1]. The hallmark of trapped lung is an inability of the lung to conform to the shape of the chest wall with the application of negative pressure in the physiologic range [1]. Therefore, pleural manometry is abnormal with an elastance of greater than 14.5 to 15.5 cm H2O/L [1]. The elastance value is the terminal slope of the pressure volume curve as pleural apposition occurs during drainage of the last remaining pleural fluid [1]. Trapped lung should be distinguished from "lung entrapment" which results from a active pleural process (inflammation or malignancy) that results in unexpandable lung following thoracentesis [1]. Trapped lung represents the end-stage of dysfunctional healing from a pleural injury that begins as a form of lung entrapment [1].
REFERENCES:
(1) Chest 2007; Huggins JT, et al. Characteristics of trapped lung. Pleural fluid analysis, manometry, and air-contrast chest CT. 131: 206-213