Year in Review, page 3
No. 8: Imaging helps unlock mysteries of dementia, Alzheimer's
In 2012, medical imaging took major strides in revealing why some people develop neurological afflictions such as Alzheimer's disease and dementia and others do not. Imaging's growing power is being harnessed as researchers try to develop therapies -- and in some cases preventive measures -- for these diseases.
Ten years ago, the only way to determine if a person had dementia or Alzheimer's disease was through autopsy. Today, physicians can visualize the disease in living individuals through an array of neuroimaging modalities, including structural and functional MRI, SPECT, FDG-PET, and most recently PET amyloid imaging, according to Dr. Cyrus Raji, PhD, a radiology resident at the University of California, Los Angeles.
"Perhaps the greatest benefit of the many brain imaging methods out there for Alzheimer's disease is the ability to see if new treatments are effective," Raji said. "While this approach has traditionally been used for drug trials, we can now see with imaging the influence of lifestyle factors and interventions on brain structure."
Over the past three years, Raji has led studies that used MRI to show how walking, eating baked or broiled fish on a weekly basis, and general everyday physical activity can reduce the risk of developing mild cognitive impairment and Alzheimer's.
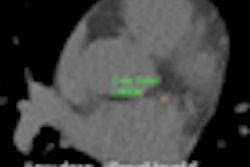
 Images show the effect on brain structure of burning calories (top, entire study group; bottom, Alzheimer's patients). Gray-matter volume increases with the amount of calories burned. Hotter colors, such as red, indicate a stronger effect. Images courtesy of RSNA and Dr. Cyrus Raji, PhD.
Images show the effect on brain structure of burning calories (top, entire study group; bottom, Alzheimer's patients). Gray-matter volume increases with the amount of calories burned. Hotter colors, such as red, indicate a stronger effect. Images courtesy of RSNA and Dr. Cyrus Raji, PhD.One of the more noteworthy events of 2012 occurred in April, when the U.S. Food and Drug Administration (FDA) cleared the radiopharmaceutical florbetapir for PET imaging to estimate beta-amyloid plaque density in the brains of patients being evaluated for cognitive impairment. Florbetapir is designed to bind to these plaques, which have been associated with the onset of Alzheimer's disease.
It was a significant advance for Alzheimer's research, as well as for Eli Lilly and its subsidiary Avid Radiopharmaceuticals, which are marketing florbetapir under the brand name Amyvid.
The next big date for Amyvid is January 30, 2013, when the U.S. Centers for Medicare and Medicaid Services (CMS) will convene an advisory committee to review its policies regarding the coverage of PET studies of beta amyloid in the brain. CMS is seeking input on whether the use of PET can improve health outcomes of patients.
"The most ambitious goal of this field is to use our neuroimaging tools to identify those most at risk for Alzheimer's disease and apply treatments before the disease progresses," Raji said. "In 10 years, we may be seeing elderly individuals getting imaging-driven 'brain checkups' for this purpose."
Who knows? It may not be long before imaging for mild cognitive impairment and dementia will be as routine as checking patients' cholesterol levels and blood pressure.
By Wayne Forrest
No. 9: 'Cheating' scandal rocks radiology board exam system
The year in radiology residency began with a bombshell: A January exposé by CNN revealed that radiology residents have for years been meticulously compiling and sharing questions, known as recalls, from old American Board of Radiology (ABR) exams given to third-year residents.
"Questions and answers have been memorized, sometimes verbatim, and contributed to extensive archives of old ABR test material that become the prize possessions of many residency programs," ABR Executive Director Dr. Gary Becker told the news network. He even went so far as to call the practice "cheating."
Radiology residents sign a document agreeing not to share test materials, but the advice has been widely ignored. ABR emphasized that archiving and sharing questions from oral board exams is unethical, unprofessional, and unacceptable.
But then a funny thing happened. Although many radiologists roundly condemned the practice, some jumped in to defend recalls as simply part of the system. After all, the thinking went, learning previously answered questions was still learning.
 Recalls stirred up trouble for residents in 2012.
Recalls stirred up trouble for residents in 2012.Radiology legal expert Dr. Leonard Berlin, vice chair of radiology at NorthShore University HealthSystem, said that while the practice of recalls may not be ideal, it is part of the system. But he cited the scandal as evidence that the ABR needed to drop its move to eliminate the oral boards, saying that it gives examiners a different perspective on a candidate's degree of knowledge and professionalism.
But that train has left the station. Right on schedule, the oral board exam will officially be retired in 2013 in favor of a completely new system for certifying new radiologists. Instead of the traditional written exams in physics and diagnostic radiology, ABR core exams will be administered as qualifying exams at the end of the third year of residency.
Beginning in 2015, residents' second test, the certifying exam, will be given 15 months after they have finished their fourth year of residency. The fourth year is seen as a chance for residents to really drill down into a specialty area, while the first through third years are envisioned as a way to learn the core competencies and take a revamped qualifying exam without the distraction or the intensity of the oral boards.
But questions remain about the new system. Private practices wonder how they're going to properly evaluate employment candidates who won't pass their final certification until 15 months after completing their fourth year of residency. Program directors are wondering how they'll balance the needs of both beginning and fourth-year residents with increasingly limited program resources.
Either way, the first of ABR's three-year core competency exams will be administered starting in September 2013, while the new fourth-year certifying exam will get its first run in 2015.
By Eric Barnes
No. 10: New iPad drives accelerating interest in mobile devices
While interest in mobile devices was already on the rise in radiology, Apple's new iPad only added fuel to the fire when it was released in March.
The third generation of the popular tablet added a number of features particularly valuable for image viewing: notably, the new Retina display that offers 2,048 x 1,536-pixel resolution at 264 pixels per inch. That's equivalent to a 3-megapixel PACS monitor and a significant improvement over the iPad 2's 1,024 x 768-pixel resolution at 132 pixels per inch.
This higher resolution allows large-format studies such as some computed radiography (CR) and digital radiography (DR) exams to be read closer to their native resolution without having to scroll around the tablet. Although mobile displays are currently considered to be too small for routine primary diagnosis, researchers are continuing to demonstrate the clinical utility of these devices in a variety of modalities and clinical situations, including with certain radiography studies.
 The new iPad's Retina display raised the tablet's resolution to the level of a 3-megapixel monitor. Image courtesy of MIM Software.
The new iPad's Retina display raised the tablet's resolution to the level of a 3-megapixel monitor. Image courtesy of MIM Software.The most powerful and prevalent use case for mobile devices in radiology, however, remains in providing referring physicians with portable access to images and related information.
Practices continue to have a number of options to choose from for their mobile image viewing needs, including dedicated apps, which have tended to provide the most functionality. Given the growing popularity of the Android platform, a number of vendors are also increasingly pursuing browser-based offerings utilizing the HTML5 standard to provide an image viewing experience that is independent of any particular software platform or device.
Concerns over mobile device security are beginning to lessen, as vendors have emphasized security features in their mobile image viewing offerings. Meanwhile, consumers are becoming more educated about the security tools included with today's mobile devices.
Mobile display quality assurance continues to be a factor, however. While a number of mobile applications have received U.S. Food and Drug Administration (FDA) clearance for diagnostic viewing in radiology in the absence of a diagnostic workstation, the agency is still determining how to regulate certain aspects of mobile devices, including their use in varying lighting conditions and even the potential effects of fingerprints on displays.
Nonetheless, in 2013 expect continued adoption of mobile devices by institutions -- and even patients -- for on-the-go access to images and reports. Also keep an eye out for innovative uses of the iPad, such as to facilitate collaboration with referring physicians, to aid cloud-based image sharing, and, in combination with motion-sensing devices, to enable interventional radiologists to review real-time intraoperative images in the interventional radiology suite.
By Erik L. Ridley