Women can safely continue antithrombotic therapy during breast core-needle biopsy, according to research published May 10 in the American Journal of Roentgenology.
A team led by Dr. Melissa Reichman from Weill Cornell Medicine at New York-Presbyterian Hospital found that frequencies of imaging-apparent and palpable hematoma are not significantly different between women who temporarily discontinue or maintain use of antithrombotic therapy.
"These results may aid the ongoing development of institutional policies and professional guidelines regarding periprocedural antithrombotic therapy management in patients undergoing breast core needle biopsy," Reichman and colleagues wrote.
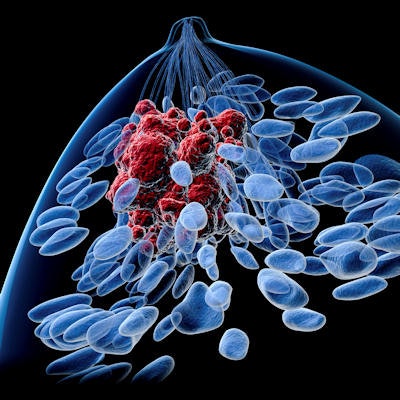
Image-guided core needle biopsy is the standard procedure for women needing tissue diagnosis for imaging-detected breast or axillary lesions. However, the researchers pointed out that there is no consensus for its use in women undergoing antithrombotic therapy, which includes medications related to antiplatelet drugs and anticoagulants.
Multiple imaging societies say that antithrombotic therapy is a relative contraindication to core needle biopsy and recommend that the decision of whether to temporarily discontinue therapy before biopsy should be determined on a case-by-case basis. However, temporarily stopping such therapy could increase the risk of significant adverse thrombotic events. The researchers also noted that coordinating the discontinuation of antithrombotic therapy may lead to delays in diagnosis and treatment.
Reichman and colleagues wanted to compare the frequency of bleeding events after breast core needle biopsy between patients without antithrombotic therapy use, patients temporarily discontinuing therapy, and patients maintaining therapy during biopsy.
It included 5,302 women with an average age of 52 years in the study. Of these, 4,665 women were not receiving therapy, 423 temporarily discontinued therapy, and 214 maintained therapy during biopsy. The women who temporarily discontinued therapy stopped five days before their biopsy appointment.
Mammograms performed immediately following biopsy for potential imaging-apparent hematoma. In addition, patients were called one to two days after biopsy and asked about palpable hematoma and breast bruise. Imaging modalities used for guidance during breast biopsy included ultrasound, mammography, digital breast tomosynthesis (DBT), and MRI.
The researchers found that imaging-apparent hematoma occurred in 3% of patients without therapy use, 6% of patients discontinuing therapy, and 7% of patients maintaining therapy (p = 0.60, discontinuing vs. maintaining).
They also found that palpable hematoma occurred in 2% of patients without therapy use, 4% of patients maintaining therapy, and 4% of patients continuing therapy (p = 0.92, discontinuing vs. maintaining). Additionally, breast bruising occurred in 2% of patients without therapy use, 1% of patients discontinuing therapy, and 6% of patients maintaining therapy (p < 0.001, discontinuing vs. maintaining).
The team also found that in multivariable analysis, discontinued therapy was not a significant independent predictor of imaging-apparent hematoma (p = 0.23), or palpable hematoma (p = 0.91). However, it did independently predict decreased risk of bruise (odds ratio = 0.11, p < 0.001). Additionally, no patient developed clinically significant hematoma after undergoing biopsy.
The study authors wrote that despite the overall safety of continuing antithrombotic therapy during breast biopsy, women who choose to do so should be informed of a greater risk of breast bruising.



















