A contrast agent should be used to improve the Doppler profile on echocardiography and more accurately measure aortic valve areas for surgical aortic valve replacement, suggests a new study in the Journal of Cardiothoracic and Vascular Anesthesia.
Researchers led by Dr. Zachary Haas from the University of Buffalo in New York found significant discrepancies between echocardiographic measures that did or did not use contrast, which could affect surgical strategies regarding the aortic valve in the heart.
"Perioperative echocardiography physicians should consider using contrast with their Doppler studies to be able to reproduce the data obtained by echocardiography cardiologists during preoperative transthoracic examinations," said corresponding author Dr. Nader Nader, PhD, from the university to AuntMinnie.com.
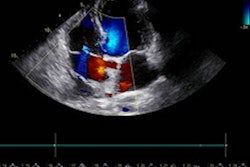
The severity of aortic valve stenosis is classified by aortic valve measurements, which includes area evaluation via transthoracic echocardiography (TTE) or transesophageal echocardiography (TEE). However, there's a discordance between the two methods; TEE "tends" to have lower maximum velocities and peak and average gradient measures than those acquired during preoperative TTE exams, according to the researchers.
"This discordance could lead to the misclassification of the severity of aortic stenosis and ultimately affect the surgical plan," the researchers wrote.
Haas and colleagues wanted to explore the level of agreement in aortic valve sizing between methods using and not using ultrasound contrast during intraoperative TEE. To calculate aortic valve area, they measured peak and average aortic valve gradients and velocity-time integral readings through the left ventricular outflow tract and the aortic valve.
The researchers looked at Doppler studies of 30 consecutive patients with an average age of 71 years who were undergoing aortic valve replacement. They took measurements before and after administering contrast. The contrast was injected slowly, appropriate gain settings were applied to the ultrasound machine, and sufficient time was allowed for contrast distribution in the left ventricle to avoid blooming.
The team found that by not using a contrast agent, the aortic valve area was overestimated by 0.26 cm2 compared to those measured by TTE (p < 0.001). However, when a contrast agent was used, TEE measurements were comparable to those obtained by TTE.
The researchers also found that without contrast, the peak and mean aortic valve gradients were underestimated by 19 and 11 mmHg, respectively (p < 0.001). Additionally, adding contrast did not affect the pulse-wave Doppler readings of V1 velocity of the left ventricular outflow tract, the team reported.
The study authors suggested that without contrast, TEE underestimates aortic stenosis severity compared with TTE or TEE with contrast. Nader said that when contrast isn't used, TEE does not produce a traceable Doppler signal, underestimating the flow velocity through the aortic valve. From there, transvalvular pressure gradients are underestimated and the area of the aortic valve is overestimated.
"The use of contrast corrects this shortcoming of the intra-operative TEE by improving the quality and visibility of the Doppler signal across the aortic valve, and makes results comparable to TTE, which is currently the gold standard for measuring the aortic valve area," he added.
The authors also noted that using contrast can allow for more repeatable measurements.
"Ultrasound contrast administration is a safe and inexpensive way to obtain valuable and accurate information about a patient's aortic valve condition," Haas and colleagues wrote. "This information can be used to aid in clinical decision-making."
Nader told AuntMinnie.com that the results of this study should be validated by larger-sized studies, and that future research could look at fine-tuning the exact dose and timing of the contrast injection.