Thyroid Cancer:
General:
I-131 scanning has been the mainstay for the evaluation of recurrent thyroid carcinoma. Patients who are found to have I-131 accumulating local recurrences or metastases on diagnostic scans will usually receive subsequent therapeutic I-131 doses which may be curative. Unfortunately, not all recurrences are iodine avid (50-60% of papillary and 64-67% of follicular cancer recurrences are iodine avid [4]). Patients with elevated human thyroglobulin levels, but negative I-131 scans pose a diagnostic and therapeutic dilemma. Although therapy with I-131 has been performed in these patients with subsequent decline in thyroglobulin levels [5], one can never be certain if all sites of disease have been adequately treated. Surgical resection of untreated sites of disease would certainly be desirable [4]. Other agents such as Tc-sestamibi, Tc-tetrofosmin, and thallium-201 have all be used to evaluate for non-iodine avid recurrent cancer and metastatic disease. Although useful for locoregional disease, physiologic accumulation of these agents in other organs (particularly within the abdomen) limits their usefulness for whole body examinations. FDG PET imaging has also shown great promise in the detection of metastatic disease in post-thyroidectomy/I-131 ablation patients [1,2]. Unlike conventional imaging, FDG PET imaging can detect metastatic disease to normal sized lymph nodes [1]. I-131 scintigraphy and FDG PET imaging are complementary diagnostic methods for the evaluation of recurrent or metastatic thyroid cancer [3,6]. The iodine uptake of a tumor is inversely related to its glucose metabolism [3]. Tumor uptake is also related to the degree of tumor differentiation [4]. In general, highly differentiated thyroid carcinoma will be I-131 positive and FDG PET negative, while less differentiated cancers will show the reverse (i.e.: FDG PET positive and I-131 negative) [1,6]. It is important to remember that although FDG-positive recurrences may indicate dedifferentiated and more aggressive tumors, this finding does not automatically predict a worse prognosis [4]. Interestingly, patients with higher thyroglobulin levels (above 100 ug/L) have been shown to have a higher incidence of true-positive FDG PET exams [4]. Another benefit of FDG PET imaging is the identification of unsuspected secondary malignancies [4].
One of the benefits of FDG PET imaging is that patients do not need to discontinue hormonal replacement therapy prior to imaging, however, one article has suggested that lesion detection is improved when performing the exam during TSH stimulation (following exogenous thyroid hormone removal) [3]. Further studies will be required to determine the optimal method for the FDG PET examination in thyroid cancer patients.
Applications for FDG PET in thyroid cancer:
Diagnosis:
FDG PET is probably not indicated for the diagnosis of thyroid cancer. Not all malignant thyroid lesions will accumulate FDG and some benign lesions will show increased metabolic activity.
Staging:
No information is currently available regarding the utility of FDG PET for the staging of thyroid carcinoma. It will likely not play a primary role.
FDG PET Imaging in Patients with Suspected Recurrent Thyroid Cancer and Negative I-131 Scans:
For the detection of recurrent thyroid cancer in patients with negative I-131 scans, FDG PET imaging has a reported sensitivity of 69-94%, and specificity of 42-95% [1,4,7]. FDG PET can detect the presence of metastatic disease in up to 70% normal sized lymph nodes [7]. Metastases to nodes as small as 4 mm have been demonstrated on PET imaging [7]. FDG PET imaging can have significant impact on patient management in this difficult subset of patients. Treatment can be changed in over 50% of patients based upon FDG PET imaging results [4]. A drawback of FDG PET imaging is that diffuse small lung metastases may not be identified and false negative exams can occur even in the presence of nodal metastases [7]. FDG PET imaging should be viewed as another tool for assisting in the detection of non-iodine avid thyroid metastases.
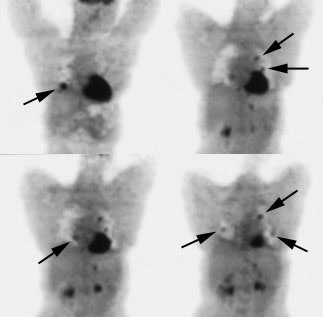
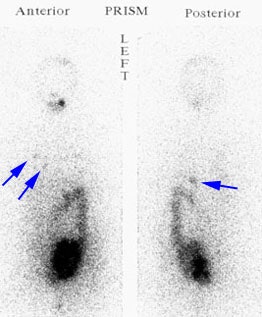
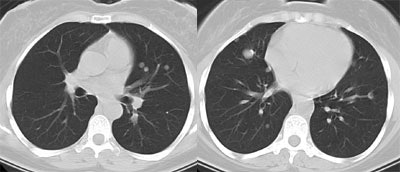
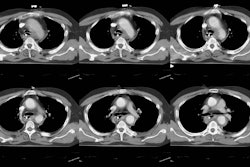
Recurrent Hurthle cell carcinoma: The patient had a history of Hurthle cell carcinoma of the thyroid. Pulmonary metastases are significantly more evident on the coincidence FDG PET examination (below left black arrows) when compared to the I131 scan (below right blue arrows). A CT scan confirmed the presence of pulmonary metastases (below). Note that a subtle bone metastasis to the high left parietal bone can be seen on I131 images. The FDG PET exam did not include this region. |
|
Non-pathologic findings:
Following thyroidectomy, FDG uptake in the thyroid bed is a common finding and does not necessarily indicate recurrent disease unless a definite mass can be identified with other imaging modalities [2]. False positive cases have occurred in association with mediastinal tuberculous adenitis.
REFERENCES:
(1) J Nucl Med 1999; Chung JK, et al. Value of FDG PET in papillary thyroid carcinoma with negative I-131 whole body scan. 40: 986-992
(2) J Nucl Med 2000; Alnafisi NS, et al. FDG PET of recurrent or metastatic 131I-negative papillary thyroid carcinoma. 41: 1010-1015
(3) J Nucl Med 2000; Moog F, et al. Influence of thyroid-stimulating hormone levels on uptake of FDG in recurrent and metastatic differentiated thyroid carcinoma. 41: 1989-1995
(4) J Nucl Med 2001; Schluter B, et al. Impact of FDG PET on patientw with differentiated thyroid cancer who present with elevated thyroglobulin and negative 131-I scan. 42: 71-76
(5) Thyroid 1994; Clark OH, et al. Managament of patients with differentiated thyroid cancer who have positive serum thyroglobulin levels and negative radioiodine scans. 4 (4): 501-505
(6) J Nucl Med 2001; Shiga T, et al. Comparison of 18F-FDG, 131I-Na, and 201-Tl in diagnosis of recurrent or metastatic thyroid cancer. 42: 414-419
(7) Head Neck 2001; Yeo JS, et al. F-18-fluorodeoxyglucose positron emission tomography as a presurgical evaluation modality for i-131 scan-negative thryoid carcinoma patients with local recurrence in cervical lymph nodes. 23: 94-103