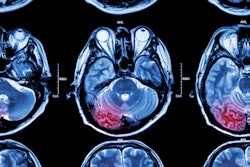
German researchers are recommending the use of diffusion-weighted MRI (DWI-MR) instead of CT to diagnose acute ischemic stroke within 12 hours of a person's first stroke symptom, according to new guidelines published in the July 13 issue of Neurology.
The study found that DWI-MR images identified stroke 83% of the time, compared with 26% for CT. DWI also more accurately detected lesions from stroke and helped identify the severity of some types of stroke, or diagnosed other medical conditions with similar symptoms (Neurology, July 2010, Vol. 75:2, pp. 177-185).
The research and recommendations come from the Johannes Wesling Clinical Center in Minden. The guidelines give doctors clear direction in using MRI first, ultimately helping people to get an acute stroke diagnosis and treatment faster, said lead author Peter Schellinger, MD, PhD.
However, one situation in which CT may still be used first is when a person needs an emergency injection of drug therapy (intravenous thrombolytic therapy) to break blood clots, if MRI is not immediately available, to avoid delays in starting this treatment, the authors noted.
Past literature
The foundation of the study came from a panel of neurologists, neuroradiologists, and radiologists who analyzed literature from 1966 to January 2008 to assess the use of DWI and perfusion-weighted imaging (PWI) in diagnosing patients with acute ischemic stroke.
To determine MRI's accuracy, sensitivity, and specificity, the group explored two questions:
- Are DWI and PWI sensitive and specific in diagnosing acute ischemic stroke, compared to concurrent imaging with other techniques, established by follow-up imaging, clinical follow-up, and final discharge diagnosis?
- Does the volume of the DWI or PWI abnormality predict initial clinical severity, final infarct size, and late clinical outcome?
For the first question, researchers used a standard 12-hour time window, since most treatment studies for acute stroke have an inclusion window of less than 12 hours. For the second question, researchers chose a 24-hour time window and excluded studies in which any patients received thrombolytic therapy so as not to confound the prognostic value of DWI and PWI.
The researchers then rated the quality of the studies, with class I indicating the highest quality and class IV the lowest. They restricted their own findings to class I and class II research, finding one class I stroke study and three class II stroke studies for DWI that fit their criteria. All PWI studies were class IV stroke studies.
Stroke studies
The class I study assessed the accuracy of DWI and MRI gradient-echo scans compared to CT in 356 consecutive patients who presented at a hospital emergency department over an 18-month period and in whom emergency physicians diagnosed possible acute stroke.
Based on the final hospital discharge diagnosis, confirmed through follow-up imaging and clinical data, DWI achieved sensitivity of 77%, compared with 16% for CT. DWI specificity was 96%, compared with 97% for CT, while accuracy of DWI was 86%, compared with CT at 55%.
One class II study prospectively evaluated 50 patients with ischemic stroke and four patients with transient ischemic attacks (TIAs), or warning strokes. Patients were randomized to receive MRI or CT within six hours of the onset of stroke. The sensitivity of infarct detection was significantly better with DWI (91%) than with CT (61%). The accuracy of DWI (91%) also outpaced CT (61%).
One other class II prospective study of 100 patients compared DWI and CT, with 29 CT scans conducted in the first six hours of stroke symptoms, followed by DWI within seven hours of stroke symptoms. (Because 39 patients received tissue plasminogen activator [tPA] to dissolve blood clots, the study was excluded for the second question.)
DWI found abnormalities and changes in 81% of the patients, compared with CT discovering changes in 66% of the patients.
'Superior to CT'
Based on the results, "DWI is established as superior to CT for the diagnosis of acute ischemic stroke within 12 hours of symptom onset," Schellinger and colleagues concluded. The diagnostic accuracy of DWI in evaluating hemorrhagic stroke "is outside the scope of this review," they added. "There was no evidence rated better than class IV to determine the diagnostic accuracy of PWI."
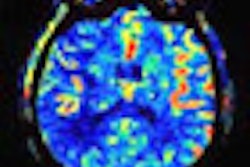
For the second question, researchers found four class IV stroke studies that evaluated a correlation between baseline DWI and PWI lesion volume and chronic lesion volume. One class II study assessed the correlation of baseline DWI and PWI lesion volume with clinical outcome. They also found two class II studies and one class III study to assess clinical and morphologic outcome.
In the class II stroke study, 115 of 631 patients (18%) had symptoms of posterior circulation ischemia. Of those 115 patients, 40 patients (34%) fulfilled the inclusion criteria with regard to the 24-hour time window and available imaging data. In all 40 patients, DWI detected an acute lesion corresponding to the patient's symptoms, while PWI detected a lesion in 16 patients.
Another class II study evaluated the use of DWI on 50 patients diagnosed with acute ischemic middle cerebral artery territory stroke (less than 24 hours after onset), while 34 patients had volumes measured by T2-weighted imaging (median 7.5 weeks after onset). The previous study found that acute lesion volumes for DWI and T2-weighted imaging correlated with the acute and chronic National Institutes of Health Stroke Scale (NIHSS) and with chronic lesion volumes.
DWI vs. PWI
In addition, one class II study examined DWI and PWI characteristics in a double-blind, placebo-controlled study involving patients with acute ischemic stroke. The study reviewed patients who received DWI and had acute ischemic stroke symptom onset 24 hours or less before the start of treatment, had NIHSS scores of 5 or higher, and had lesions of 1 mL to 120 mL in cerebral gray matter.
Of the 100 patients enrolled in this class II study, 81 patients had interpretable MR measurements. Baseline DWI and PWI lesion volumes correlated with baseline NIHSS scores. Baseline DWI volume also correlated with follow-up lesion volume 12 weeks after the stroke.
Based on the results, the authors found "significant correlations" between lesion volumes and clinical measures, and suggested that the findings support the role of DWI "as a clinically meaningful surrogate marker in stroke clinical trials."
Future research
"Evidence from our report demonstrates that DWI is accurate and superior to CT for the diagnosis of acute ischemic stroke relative to clinical and imaging outcomes," Schellinger and colleagues concluded. "However, in clinical practice, the availability and cost of imaging modalities and the requirements of medical management enter into the decision about which test to perform in the acute period."
As for future research, the authors advocated the need for prospective studies to further investigate the diagnostic capability of perfusion-weighted imaging in stroke patients and the integration of clinical and laboratory data with DWI, MR angiography, and PWI to better diagnose and predict outcome.
In addition, they recommended additional research to determine the predictive value of DWI-derived lesion volumes within the first hours of stroke and the potential added value of PWI measures to address cost-benefit issues.
By Wayne Forrest
AuntMinnie.com staff writer
July 12, 2010
Related Reading
Volume helical shuttle CT perfusion identifies stroke patients, April 20, 2010
Resting fMRI exam may predict stroke and brain injury outcomes, March 30, 2010
MRI links silent stroke to kidney failure in diabetics, February 1, 2010
MRI and CT findings comparable in stroke patients, March 9, 2007
Relative threshold method correlates CT, MRI stroke infarct assessment, February 9, 2007
Copyright © 2010 AuntMinnie.com