The adoption of PACS has improved the productivity of radiologists when reading CT exams, but there are still barriers to surmount in order to wring full efficiency gains from digital image review, according to Dr. Jeffrey Mendel from Tufts University.
For example, CT radiologists need to make sure their PACS software is integrated with a variety of information systems and that they're using all of its capabilities. New software can also help target big time sinkholes, Mendel said.
He spoke during a session at the recent International Symposium on Multidetector-Row CT in Washington, DC.
PACS gains
PACS so far has largely eliminated lost films, alternators, and paper cuts, Mendel said.
It has also provided "anywhere/anytime access [to images], assuming that you have sufficient IT support and resources to maintain your systems and keep them integrated and progressing," he said. "For a lot of medium and small-sized hospitals these days that's an enormous challenge."
Speech recognition technology has eliminated transcriptionists and cut down on wet readings and phone calls for reports. However, reports are still mainly "text blobs," making searches problematic. Without using natural language processing technology, searches for "lung cancer" yield results that include "lung cancer" as well as "no evidence of lung cancer" and miss, for example, "bronchogenic carcinomas," he said.
Quality improvement workflow is here, but it's uncertain whether it will be a boon to radiologist productivity or instead will suck more time out of radiologists' days, he said.
What's wrong with PACS
A number of problems persist in PACS today, including how to find significant prior studies. This involves either scrolling through studies during a manual search or using an automated method that may still involve some scrolling.
"If you're scrolling a little, that means you don't trust your automated search, which means you don't really use it," he said.
Another issue is how to find significant pertinent patient history, he said.
In the "good" old days of radiology, film jackets had little summaries written next to each exam, providing a quick assessment of the patient's medical situation. This allowed for easy recognition when there was a significant medical/radiologic event, Mendel said.
Clinicians also used to come to radiology for consultation and review of studies, and occasionally they gave clinical history that wasn't on the imaging requisition. Now, radiologists often have to infer a patient's clinical history, he said.
Less than efficient workflow
Nor is workflow as efficient as it could be. For example, current workflow for evaluating a solitary pulmonary nodule near a lung base involves the following steps:
- Scroll to find prior CTs of the chest, abdomen, and thoracic spine; MRIs of the chest or abdomen; PET/CT; and perhaps breast MRI.
- Read prior reports for additional history/findings.
- Open each study to view series.
- Find series with lung images.
- Load specific series.
- Scroll through to find similar levels.
- If present previously, measure lesion.
- Dictate measurements and type and date of priors reviewed into the report.
- Call ordering physician and document communication.
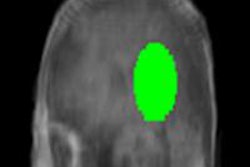
"This [workflow] is not where we want to be," Mendel said. " 'Smart' workup could really help us. Theoretically, the capability is out there for us to click on a lung base on a PACS and say 'find this,' and the PACS goes out and pulls up a hanging protocol showing all the images of a lung base aligned on a lung window, so we can look at them. And more importantly, in the background the [computer-aided detection (CAD)] system is running to measure those nodules."
Then, all of that comparative data would get into the report, which is linked to the images so that they can be easily viewed.
"Lastly, if you're dealing with a lung nodule, you've got something going on in the electronic medical record that's looking to see if this patient has ever seen a pulmonologist, and their name gets tacked onto the report," he said.
Why don't radiologists already have this?
Radiologists don't have these capabilities right now because of integration, cost, and focus. For example, the workflow example given above would require seven or eight different software systems tied together, Mendel said.
"If you don't have really strong IT support and some forward thinking, you're not going to get there," he said.
Another issue is how PACS vendors can get paid for these significant but incremental advances.
"If I have a great software program that saves radiologists and their productivity and they're not hospital-based, why is the hospital administrator going to buy it?" he asked. "Second, if a hospital has great software that's going to improve their outcomes and improve their reimbursements but decrease our productivity, why are we going to support it?"
Regarding focus, competing vendors may focus on slightly different things, and hospital IT staff may not prioritize radiology integration, Mendel said.
Big data
Another obstacle is that much information lies buried away in big data. For example, radiology reports have prior clinical history, significant radiologic findings, and measurements of lesion size. Even more good stuff is available in the electronic medical record, including the name of the primary care provider and specialist, clinical history and previous diagnoses, and clinically relevant lab values and pathology results, according to Mendel.
Two concepts are important for accessing this information: natural language processing, which uses computers to pull out the data, and ontology, which deals with what entities exist and how entities can be grouped and related, he said.
It's also important to embrace structured reporting, which helps radiologists view old reports and more quickly interface reports with clinicians and data.
Structured reports can more easily be linked to PACS measurements. Software can assign specific descriptions to anatomic categories within structured reports, according to Mendel.
Productivity equation
Productivity equals time minus mouse clicks, Mendel said. This means it's important to buy intuitive/adaptable PACS software that promotes the use of a single set of keyboard shortcuts and mouse actions.
CT radiologists need to take three steps to improve productivity, he said. First, they should ask if their current software is really integrated. Next, they should ask if they are using all of the capabilities of their current software. The last step is to buy more software.
For this process, radiologists should determine their greatest time sinkholes and any hospital-wide goals they can tie into. Then, find out what software is available and most easily integrated and adaptable, he said.
In addition, Mendel emphasized that if you are in a department that is considering a replacement PACS, speech recognition system, or RIS, make sure that someone from CT is involved. A detailed list of necessary functionality should be created.
It's also important to obtain written confirmation from any vendors about their current software capabilities, integration capabilities, workflow adaptability, and software in development and release dates, Mendel said.
"Everybody needs help reading CT," he concluded.