AI in breast cancer screening is not cost-effective despite “modest” reductions in mortality, according to research published September 20 in Value in Health.
A team led by Ilana Richman MD, from Yale University in New Haven, CT, found in its microsimulation study that AI led to slightly lower mortality compared to digital breast tomosynthesis (DBT) alone. However, AI was not cost-effective at a willingness-to-pay threshold of $100,000 per quality-adjusted life year (QALY) due to increases in ductal carcinoma in situ (DCIS) diagnoses.
“We anticipate that even if AI resulted in greater improvements in performance by providing larger gains in accuracy in real world settings, AI still may not be cost effective at the current price,” the Richman team wrote.
AI assistance leads to improved diagnostic accuracy in breast cancer screening, according to recent studies. However, the researchers noted that the long-term health outcomes and cost-effectiveness of AI-assisted screening are not well known.
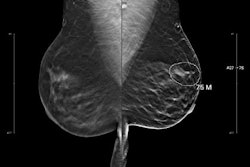
Richman and colleagues estimated benefits, harms, and cost-effectiveness of incorporating an AI product, Saige-DX, into standard screening with DBT. They developed a microsimulation model using data from Surveillance, Epidemiology, and End Results (SEER), the Breast Cancer Surveillance Consortium (BCSC), and published data on AI performance.
The model compared DBT alone with DBT plus AI in biennial screening for women ages 40 to 74 years. The study included a cohort of 1,000 women from the data.
The team reported the following findings:
AI-assisted screening reduced false-negative screens by 2.1 per 1,000 women and false positives by 50 per 1,000 women.
AI-assisted screening resulted in 0.33 fewer advanced breast cancer cases (regional or metastatic cancer) per 1,000 women at diagnosis and 0.13 fewer breast cancer deaths per 1,000 women compared to DBT alone.
Screening with AI resulted in 3.09 additional QALYs and an increase in lifetime costs of $936,430 per 1,000 women. This led to an incremental cost effectiveness ratio (ICER) of $303,279 per QALY.
The team also found that AI was not cost-effective at a $100,000/QALY willingness-to-pay threshold in 98% of simulations.
AI-assisted screening led to a 21% increase in DCIS. The researchers suggested that DCIS diagnosis “was a key driver of cost and likely contributed to our finding that AI is not cost effective even at very low prices.” Using the $100,000/QALY willingness-to-pay threshold, AI could not achieve cost-effectiveness at any price due to incremental cost associated with DCIS detection. When priced at five dollars, AI was cost effective in only 36% of trials, the researchers highlighted.
“Findings were not sensitive to changes in test characteristics likely to be observed in routine practice,” they added.
The team called for long-term studies to evaluate the impact of AI-assisted screening on DCIS diagnosis, overdiagnosis, and breast cancer outcomes.
Read the full study here.