Computer-aided detection (CAD) technology for mammography has become increasingly accepted and refined since it was introduced nearly 20 years ago. But the clinical community continues to debate the technology’s effectiveness under widely varying clinical conditions. Of particular concern is whether CAD results are reliably reproducible, and whether CAD for mammography increases recall rates with a high incidence of false-positive results. Two recent studies addressed these issues.
Improvement in reproducibility rate
Researchers from the departments of radiology at the University of Pittsburgh and Magee-Women’s Hospital in Pittsburgh found that the reproducibility of CAD results has improved, in part because false-positive detection rates have been reduced as the technology has been refined.(Radiology Online, May 20, 2003).
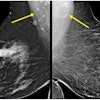
Bin Zheng, Ph.D., and colleagues used 100 mammographic cases with four views each from a database of more than 1,000 digitized images and diagnostic results. The cases were chosen by a staff member not otherwise involved in the study, and included 25 with microcalcification clusters and 75 with masses; two-thirds were cases that had been confirmed as malignant.
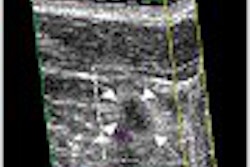
Zheng and colleagues used R2 Technology’s ImageChecker version 2.0 to scan the images three times over a period of three weeks. If the CAD unit’s marking was anywhere inside a true-positive area in the image, the mass was regarded as correctly identified by the system. Likewise, if the system’s marking overlapped any of the microcalcification areas, it was considered true-positive.
The group assessed the sensitivity, false-positive rate, and reproducibility of the ImageChecker for abnormality- and region-based values. Abnormality-based sensitivity for mass detection ranged from 66.7% to 70.8%. ImageChecker identified 48 of 50 microcalcifications on all three scans. Mass detection for region-based sensitivity ranged from 51.0% to 52.6%, while region-based sensitivity for microcalcification clusters ranged from 85.0% to 87.0% for individual cluster regions and 85.5% to 87.1% for malignant clusters.
ImageChecker produced identical results for 213 of 400 images, increasing overall reproducibility to 53.3%, up from 38.5% found in a study published in 2000 (European Journal of Radiology, December 2000, Vol.36:3, pp.170-174).
Zheng and colleagues posited that this improvement could be due mainly to a decrease in the system’s false-positive rate as its software has been refined, from 1.0 to 0.5 per image, according to a study by Dr. Ronald Castellino and co-authors presented at the 2000 RSNA meeting in Chicago.
The reproducibility rate for true-positive areas was higher than for false-positive areas. For true-positive mass regions of interest, the system generated 118 cues in three scans, 82 (69.5%) of which were marked at the same locations.
Reproducibility for false-positive regions was lower, with only 44.0% of mass regions and 31.9% of microcalcification cluster areas marked at the same location in all three CAD scans.
Zheng and colleagues suggested that the sensitivity for the detection of microcalcification clusters is high and, as a result, the reproducibility of results is also high, making CAD a useful tool for use during the diagnostic process.
Improvement in recall rates
One of Zheng’s colleagues, Dr. Laura Hardesty of the University of Pittsburgh School of Medicine, presented results from another study performed in her department at the 2003 American Roentgen Ray Society conference in San Diego.
The study was conducted during two eight-month periods: July 2000 to February 2001 (without CAD) and July 2001 to February 2002 (with CAD). Using MQSA audit data, Dr. Hardesty and colleagues found the number of screening mammograms interpreted and the number of patients recalled for further imaging on a monthly basis for each of the department’s eight breast imaging subspecialists for these periods.
The group also calculated the percentage of screening mammograms recalled for additional imaging, both for each of the eight specialists and for the radiology group as a whole.
"We excluded the period of March 2001 through June 2001 as a training period when we were becoming used to using the CAD and seeing how it affected our results," Hardesty explained.
The group interpreted 19,335 screening mammograms during the first time period, without the help of CAD, and 17,598 during the second time period, using CAD (R2’s ImageChecker). The difference between recall rates for the group on the whole without use of CAD and with the use of the technology was marginal: 11.6% and 11.1%, respectively.
These results stand out against a study by Drs. Timothy Freer and Michael Ulissey, which found a 19% increase in recall rate when CAD technology was used, but confirms a study lead by Dr. Linda Warren-Burhenne that also found no increase in recall rate with CAD use (Radiology, September 2001, Vol.220:3, pp.781-786; Radiology, May 2000, Vol.215:2, pp.554-562).
These findings suggest that CAD’s highly-publicized increase in breast cancer detection rates (ranging from 10% to 30% more cancers found) will be even more relevant if there is not a statistically significant, associated increase in recall rates, Hardesty said.
ARRS session moderator Dr. Barbara Monsees asked Hardesty if the use of CAD had an impact on the length of interpretation time.
"We didn’t actually time it for study purpose but in those first several months when we were utilizing it, there was a lot of frustration expressed by the breast imagers that it was taking longer," Hardesty replied. "I definitely was in that group. I would say that I held on to the frustration longer than the rest of my colleagues. But the more you use it, like any other tool, you slip into a pattern. At this point, I do not think that it takes any longer with CAD."
Additional reporting by Shalmali Pal.
By Kate Madden YeeAuntMinnie.com contributing writer
June 30, 2003
Related Reading
Computer-aided detection enhances breast MRI, June 6, 2003
Effective breast CAD still harbors a few workflow caveats, June 3, 2003
CAD mass markers aid in reduction of mammographic interpretation errors, March 7, 2003
Researchers compare CAD systems for mammography, December 6, 2002
Copyright © 2003 AuntMinnie.com