Diverticular disease is all too common in Western countries, where low-fiber diets and processed foods still rule despite resounding calls for better eating habits. Estimates are that close to half of all Americans over 50 suffer from some form of the disease. And since this age group is precisely the colorectal cancer screening population, it's inevitable that some of these folks will end up having virtual colonoscopy.
Yet no one had really evaluated the appropriateness of virtual colonoscopy in these patients, so Dr. Marc Gollub and colleagues from Memorial Sloan-Kettering Cancer Center in New York City decided to do so. They found that muscular hypertrophy, a pathology present in some diverticular disease, can significantly limit the diagnostic value of virtual colonoscopy. In April, Gollub presented the preliminary findings of an ongoing study at the International Symposium of Virtual Colonoscopy in Boston.
"(Muscular hypertrophy) is primarily a muscular disorder which has been termed myochosis, which consists of deposition of elastin in a longitudinal taenia muscle, and subsequent shortening and bunching up of the circular muscle," Gollub said. "This may even predate the formation of diverticula."
The condition is most common in the sigmoid colon, where it narrows the colon lumen and creates the highest intersegmental pressure, Gollub said, describing features that were elucidated in a 1967 study by Williams et al (Radiology, September 1967, Vol. 89:3, pp. 401-12).
Since diverticular disease is known to occasionally interfere with colonoscopy, Gollub's group sought to assess the quality of virtual colonoscopy exams in patients with diverticular disease, and compare it to VC results obtained in patients without diverticular disease.
In all, 99 patients (35 men, 64 women, mean age 64) participated in the study, including 82 who were referred following incomplete colonoscopy, 26 with diverticula at colonoscopy, and 6 in whom diverticular disease explained the failed colonoscopy. Nine were excluded for neoplasms.
The subjects underwent virtual colonoscopy following a phospho-soda prep. All patients received 1 mg of glucagon and 30 to 65 pumps of room-air insufflation. Three radiologists (two at a time), reviewed a total of 100 VC exams in 2-D on a PACS workstation. They assessed the severity of diverticular disease based on the number of diverticula, or "tics" (Grade 1, 1-10; Grade 2, more than 11).
"In the area of diverticula, we evaluated for muscular hypertrophy or spasm or benign segmental wall thickening," he said, qualitatively rating each of 8 colon segments from rectum to cecum (1=collapsed, 2=minimal, 3=good, 4=optimal). A grade of 4 represented complete defacement of the haustral folds and excellent distension, Gollub said. In addition, quantitative ratings were made of the luminal diameter of the sigmoid region from inner wall to inner wall (maximum, minimum, and average).
"We excluded (9) patients who had narrowing from known malignancy," he said. Forty of 100 exams showed diverticular disease, with the incidence fairly evenly divided between patients with 1-10 tics (19) and those with more than 11 tics (21). Patients with 11 or more tics were slightly more likely to have myochosis (13/21) than patients with 10 or fewer tics (8/19), but the difference was not deemed statistically significant. Seven patients had myochosis without diverticula (tics), "which supports the hypothesis that (myochosis) may predate the formation of diverticular abnormalities," Gollub said.
Mean colonic distension was only slightly lower in patients with tics (6.16 mm) compared to those without tics (8.5 mm), and the results were similar in the sigmoid colon. However, mean sigmoid distension was dramatically smaller in patents with myochosis (4.2 mm) compared to patients without myochosis (9.04 mm).
Gollub noted a few limitations in the study’s methodology, which relied on subjective measurements of the largest and smallest diameters rather than more elegant computed measurements such as cross-sectional area, moving sphere, and selective volume measurements. In addition, terms such as hypertrophy, spasm, and benign segmental wall thickening were made without strict definitions.
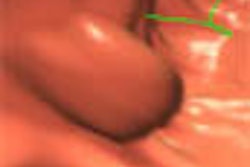
The presence of myochosis can make it difficult to distinguish muscular disease from neoplasm, whether in 2-D or 3-D views, he said. For example, if the 3-D view shows a bulging mass in the lumen that can't be identified on CT, sometimes evaluation can be made using double-contrast barium enema "by characterizing the area as a more gradual contraction without proof of any borders, and, more importantly, in the preservation of the mucosa," he said. "This is one of the few times where we think CT shows us too much information and confuses us."
 |
| Top left: prone oblique CT scan of pelvis during virtual colonoscopy showing muscular thickening in sigmoid colon. Top right: multiplanar reformatted image through muscle abnormality (myochosis) simulating a mass. Bottom left: Virtual colonoscopic view of "mass." Bottom right: double-contrast barium enema shows that "mass" is only spasm. Images courtesy of Dr. Marc Gollub. |
"Myochosis is a morphologic feature of diverticular disease which limits the quality of virtual colonoscopy in the sigmoid colon," Gollub said during his presentation. "Patients with myochosis, with or without diverticula, displayed significantly less sigmoid distension. So we feel that in patients with diverticular disease with myochosis, evaluation of the sigmoid may be limited on VC, and if patients had an incomplete colonoscopy, for example, maybe they should get another test such as the double-contrast barium enema. But VC is still an appropriate examination to look at the remainder of the colon."
Speaking later with AuntMinnie.com, Gollub described the difficulties inherent in classifying aspects of diverticular disease with CT.
"The study showed that it's not the mere presence of diverticula that accounts for the statistically lower mean minimum diameter of the sigmoid colon in patients who had diverticula -- so it must be something else," Gollub said.
What's known about diverticular disease is that it's a muscular disorder, he said. Histologically, myochosis is neither true hyperplasia nor true hypertrophy, but rather a deposition of elastin in the longitudinal fibers that foreshortens the colon like an accordion, bunching up the circular muscle fibers.
And since the study showed that it wasn't the diverticular disease that accounted for the statistically significant difference in sigmoid diameter, it must have been the muscular hypertrophy, Gollub said, noting the circularity of his argument.
What's important is that VC can be difficult in patients with diverticular disease, he said. "So why not send them for another test like DCBE?"
By Eric Barnes
AuntMinnie.com staff writer
June 20, 2002
Copyright © 2002 AuntMinnie.com