Researchers from Austria have used the saline flush to increase contrast enhancement in both parenchymal and vascular structures of the abdomen. Well known in MRI, the procedure has not been routinely used in CT, where it could potentially improve enhancement while reducing the associated costs and risks.
A saline flush after contrast administration, common in MRI exams, can prevent the pooling of contrast material in the arm veins and injection system. But the technique has not been used widely in CT, where it could potentially improve contrast enhancement and reduce the amount of contrast required, minimizing costs and the risk of allergic reaction.
Now, researchers from Austria have used the saline flush to increase contrast enhancement in both parenchymal and vascular structures of the abdomen. Dr. Helmut Schoellnast, Dr. M. Tillich, Dr. H.A. Deutschmann, and colleagues from University Hospital in Graz examined the saline-flush technique in CT exams of 41 patients.
"The aim of this study was to determine if a saline-solution flush following low-dose contrast material bolus improves parenchymal and vascular enhancement during abdominal ... MDCT," they wrote in the online edition of European Radiology (Oct. 18, 2003).
The injection of bolus contrast is generally considered to improve the visibility of hypovascular tumors by maximizing the difference in enhancement between the tumor and the organ, they wrote, adding that nonionic contrast material is preferable because it is better tolerated by patients. The high cost of such agents, however, means that it is important to keep the dose as low as possible, which also serves to reduce the risk to the patient.
The study looked at 41 patients (24 and 17 women, mean age 49) who had previously undergone contrast-enhanced abdominal CT without a saline flush, and were now undergoing MDCT follow-up with the flush (153 ± 93 days, range six to 372 days) after the first exam. None of the patients' weight had changed substantially. The indications were gastrointestinal neoplasms (n = 13), primary liver tumors (n = 10), genitourinary neoplasms (n = 4), gallbladder adenoma (n = 1), cholecystitis (n = 1), liposarcoma (n = 1), Crohn's disease (n = 1), tuberculosis of the bone (n = ), liver abscess (n = 2), pancreatitis (n = 4), and diverticulitis (n = 1), the authors wrote.
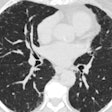
CT images were acquired from the diaphragm to the aortic bifurcation, 70 seconds after contrast administration. The researchers used a LightSpeed QX/i scanner (GE Medical Systems, Waukesha, WI), and collimation of 4 x 5 mm, 5-mm section thickness, rotation time of 0.8 sec, 120 kVp, and 200-300 mAs. An 18-F intravenous catheter was used to inject the contrast material, 300 mgl/ml iomeprol (Gerot Pharmaceuticals, Vienna) in an antecubital vein at 2.5 mL/sec, using a single-syringe power injector for the original exams. The only acquisition differences in the follow-up study were the use of a double-syringe power injector for the contrast rather than a single-syringe power injector, and the addition of a 20-mL saline-solution flush following contrast administration in the follow-up exam.
Corresponding slices of the original and follow-up images were examined side by side on a MagicView 1100 workstation (Siemens Medical Solutions, Erlangen, Germany), in regions of interest of 1-2 cm in parenchyma, and the whole vessel diameter in vascular structures. Mean enhancement and standard deviation were also evaluated quantitatively for each organ and vessel to gauge the difference between the two protocols. The Kolmogorov-Smirnov test for assessing normal distribution and Levene's test for assessing homogeneity of attenuation variants were also performed.
According to the results, there was a statistically significant difference in the amount of parenchymal and vascular enhancement when the saline-solution flush was employed.
"The mean parenchymal enhancement was 8 ± 12 HU higher with (the) double-syringe power-injector protocol," the authors wrote. "There was no significant difference in mean enhancement along the z-axis for the parenchymal organs for both protocols. With the single-syringe power-injector protocol, the mean enhancement of the superior liver segments was 106 ± 12 HU, of the inferior liver segments 105 ± 11 HU (p = 0.123). The corresponding enhancement values were 105 ± 12 and 106 ± 12 HU for the superior and inferior pole of the spleen (p = 0.199) and 150 ± 27 and 151 ± 26 HU for the superior and inferior pole of the kidneys (p = 0.451). With the double-syringe power-injector protocol, the corresponding enhancement values were 115 ±15 and 113± 13 HU for the liver (p = 0.128), 112 ± 13 and 114 ± 15 HU for the spleen (0.120), and 159 ± 26 and 160 ± 31 HU for the kidney (p = 0.316; fig. 2).
Assuming an average attenuation of unenhanced liver parenchyma of 60 HU, enhancement was more pronounced after saline flushing (54 ± 14) than without flushing (45 ± 11 HU). Moreover, hepatic enhancement was adequate in 61% of patients with flushing compared to 32% without flushing, the authors wrote.
Previous studies have shown that a minimum of 26-30 g of iodine is needed for adequate parenchymal enhancement, the authors wrote. The advantages of a saline flush in contrast enhancement can be used to compensate for dose reductions, and could reduce the risk of missing hypovascular and hypervascular lesions in the abdominal organs.
"A statistically significant improvement of 8 HU was achieved by flushing a 100-mL contrast-material bolus with 20 mL saline solution," they wrote. "Consequently, the decrease of parenchymal enhancement resulting from contrast material dose reduction ... could be partly compensated by flushing with saline solution...An increased aortic enhancement of 10 HU, as achieved in our study, may improve the detection of dissection flaps, thrombotic material, and atherosclerotic soft plaques in the abdominal aorta and its branches; however, a positive effect of saline flush on vascular enhancement may be more clinically relevant in abdominal CTA."
By Eric BarnesAuntMinnie.com staff writer
November 6, 2003
Related Reading
High pitch, thin sections can optimize MDCT protocols, August 22, 2003
Ask questions to optimize MDCT protocols, July 11, 2003
Copyright © 2003 AuntMinnie.com