PHOENIX - CT is nearly ideal for selecting patients for recanalization therapy, according to a presentation Saturday at the International Stroke Conference, sponsored by the American Stroke Association.
"Clinically, our goal is to create a multivariable model where we can get a simple set of rules or score as to who to treat, and who not to treat, with tPA (tissue plasminogen activator)," said Dr. Michael Lev, associate professor of neurology at Harvard University Medical School in Boston. "Most of what you do with MRI you can do with CT, except for the detection of small brain stem infarcts, lacunar infarcts, and microbleeds. We are not arguing that CT is better, but what we are saying is that if you don't have rapid access to an MR scanner, then doing functional CT will be better than not doing it." Lev also is a staff neurologist at Massachusetts General Hospital, also in Boston.
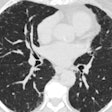
During his talk, Lev presented CT images of a patient who came in 90 minutes after onset of a right hemispheric cerebral event with a dense M1. The unenhanced CT scan was completely normal.
"When you see a CT scan that is normal, or with only subtle hypodensity, these very early hypodensities may represent a blood-pool hematocrit effect. Of course, this corresponds on an MR to a dense flare sign. So this is something you could see on MR or CT," he said.
Once CT indicated the clinical situation, the patient underwent CT angiography (CTA) to get more information about how to manage treatment. "The unenhanced CT in this patient was fairly normal," he said. "The enhanced CT shows some lack of blood pool, some lack of contrast filling. From our work so far, we believe that this could be a diffusion-weighted image (DWI) equivalent in CT imaging."
The advantage of CTA over MR angiography is cleaner, more definitive images, Lev said, especially if a 4-16 slice multidetector scanner is used. Lev said his CT protocol is a uniform, 25-second delay of biphasic injection of 90-140 ml of nonionic contrast. Lev said that making quantitative cerebral blood volume-cerebral blood flow (CBV-CBF) maps is "definitely possible" with CT.
"Unlike with MRI, and because of the linearity of the tissue dose response of the density of the contrast, we can actually get these maps to be quantitative," Lev said. "What I want to argue is that the degree of indicated CBV-CBF mismatch can be used in a way analogous to the idea of DWI-PWI (perfusion-weighted imaging) mismatch, that CT-CBV is a DWI-like measure. Of course, we need a large prospective series to validate this."
The CBF and mean transit time (MTT) maps in Lev’s example showed a large area of potential disturbed-flow tissue at risk. CBV abnormality corresponded closely to the CTA axial source images. The patient had a large area of CBF abnormality and poor collaterals. The patient was treated with intravenous thrombolysis but the treatment was not successful, Lev reported.
Three days after initial scanning, the infarct size correlated to the area that was at risk based on the CBF and MTT maps. The patient had a poor imaging and clinical outcome, Lev said. "In the absence of early, complete recanalization, regions with severe and prolonged CBF reduction will suffer infarct. The threshold, of course, is time-dependent, but, roughly speaking,beyond the 3-hour time window you are talking about at least a 50% reduction in CBV."
The size of the CBV on the CT can aid in patient risk assessment for tPA treatment, he concluded. The CT scan can be used to exclude patients most likely to hemorrhage, or include those who would benefit from tPA and an extended IV thrombolysis.
If the CBV and CBF lesions match, then there is not really a lot of area at risk, and such a patient might be a poor choice for treatment regardless of the lesion size, Lev said. "Certainly anything greater than one-third the middle cerebral artery (MCA) territory in a CBV lesion, about 100 ml in volume, is something not to treat because you already have a big area at risk. Small CBV, however, with a very large CBF penumbra would indicate a best candidate for treatment," he said.
However, CT does have some limitations. "When you are measuring the penumbra you are really only getting four 5 mm or two 10 mm contiguous slices for a given 40-50 ml bolus of contrast. But of course, you could compute quantitative CBV, CBF, and MTT from that," Lev said. But if the patient has a small lacunae and is doing well, CT imaging can help the clinician decide if he would be better served by 24-hour observation rather than immediate treatment.
"All of this imaging can help in this kind of decision-making," he said. "CT is fast and it's available. The availability is probably one of the biggest factors in getting small community hospitals involved in a teleradiology network."
When a smaller hospital in the Boston area treats a stroke patient "they will do our CTA protocol...if there is a proximal large vessel thrombus indicated over teleradiology, the helicopter will start the IV thrombolysis and get the patient over to Massachusetts General Hospital immediately," he added.
By Bruce SylvesterAuntMinnie.com contributing writer
February 17, 2003
Related Reading
Brain abnormalities on MRI seen after coronary bypass surgery, December 31, 2002
Diffusion-weighted MRI better than CT in stroke diagnosis, September 23, 2002
CT zeros in on brain-tissue damage in heat-stroke patients, August 14, 2002
Copyright © 2003 AuntMinnie.com